Clinical Correlation of Periodontal Disease Parameters with Crevicular Blood Glucose Levels
OBJECTIVE: The purpose of the study was to assess relationship between the clinical periodontal parameters and gingival crevicular blood glucose levels and to determine the relation of severity of periodontitis with glycemic levels.
METHODOLOGY: A total number of 348 patients with chronic periodontitis participated in this cross-sectional study. After recording the number of teeth and plaque percentage, the participants were assessed for severity of periodontitis according to clinical periodontal parameters of periodontal pocket depth, gingival recession, clinical attachment loss and gingival bleeding. Gingival crevicular blood glucose was assessed via glucometers and random blood glucose levels were recorded for each patient. SPSS version 20 was used for data analysis. The correlation between periodontal parameters and glycemic levels was assessed via Pearson's correlation coefficient. Multiple regression analysis was used to predict the association of glycemic levels with periodontal parameters. Analysis of variance was used to compare the glycemic levels in patients with mild, moderate and advance periodontitis.
RESULTS: Age, bleeding on probing and clinical attachment loss showed significant positive correlation while number of teeth showed significant negative association with crevicular blood glucose levels. Multiple regression analysis indicated that crevicular blood glucose has significant linear association with bleeding on probing and clinical attachment loss. Gingival crevicular blood glucose levels were found to be increasing with severity of periodontitis. There was significant difference (p<0.001) in mean glucose levels between mild, moderate and advanced periodontitis groups.
CONCLUSION: Clinical periodontal parameters and severity of periodontitis are strongly associated with increasing gingival crevicular blood glucose levels.
KEYWORDS: Blood glucose, inflammation, gingival bleeding, periodontitis
HOW TO CITE: Saeed Q, Memon S, Hosein M, Ikram S. Clinical correlation of periodontal disease parameters with crevicular blood glucose levels. J Pak Dent Assoc 2021;30(1):12-17.
DOI: https://doi.org/10.25301/JPDA.301.12
Received: 16 July 2020, Accepted: 19 September 2020
INTRODUCTION:
Chronic Periodontitis is an inflammation of the tissues supporting the teeth, caused by a variety 76 of microorganisms, leading to periodontal ligament destruction and alveolar bone loss.1The chronic tissue damage is caused by bacterial by-products and inflammatory response produced by the host. Altered immune response
and compromised immunity also plays an important role in this destructive process.2
The major contributors to this compromised immunity are systemic diseases like diabetes mellitus, cardiovascular disorders and respiratory diseases, which are some of the known risk factors for periodontitis.3 Diabetes mellitus demonstrates a bidirectional relationship with periodontal inflammation. Past investigations suggest that periodontitis is progressively pervasive in patients with poorly controlled diabetes.4-6
Increased glycemic levels in diabetes leads to the production of advanced glycation end substances (AGEs), which compromise the capability of repair in periodontal tissues and favors periodontal inflammation.7
While chronic periodontitis negatively impacts diabetes by affecting the action of insulin and causes insulin resistance which worsens the metabolic condition.8 It has been reported that mechanical debridement of plaque and calculus in patients with periodontitis and maintaining adequate periodontal health, assists with controlling the periodontal inflammation and lowering the levels of HbA1c over the span of 6 months.9
The clinical parameters indicating chronic periodontitis include gingival bleeding while probing (Gingival crevicular blood) and clinical periodontal attachment loss of more than 3 mm.10 The diagnosis according to severity is made according to the degree of clinical attachment loss and periodontal pocket depth.11 Many studies have linked periodontal disease with diabetes but there is still not enough literature available on the relationship between clinical parameters of periodontitis and gingival crevicular blood glucose levels. Therefore, the objectives of the study were:
- To find the correlation between clinical periodontal attachment loss (CAL), gingival bleeding on probing, plaque percentage and tooth loss with crevicular blood glucose levels of the patients with chronic periodontitis.
- To predict the association of various periodontal parameters with gingival crevicular blood glucose levels
- To evaluate the difference in gingival crevicular blood glucose values in mild, moderate and advanced periodontitis patients.
METHODOLOGY:
The cross sectional study was conducted for the term of 6 months beginning from January 2019 to June 2019, among patients with periodontitis, visiting the department of Oral Medicine, Ziauddin Dental Hospital, Karachi. The study was accepted by Research Advocacy Committee, Ethical Review Committee and Board of Advanced Studies and Research Ziauddin University, under the reference number 0450818QPOM. Open Epi Version 3.0 was used to obtain the sample size of 348 participants, which was calculated according to 34.5% prevalence of periodontitis in Pakistan and 95% confidence interval.12 Male and female patients aged between 25 to 60 years, presenting with periodontitis (>3 mm clinical attachment loss and bleeding on probing) were included in the study, whereas, the exclusion criteria was history of hematological, cardiovascular, renal and hepatic diseases and the presence of purulent periodontal discharge.
After obtaining an informed consent and demographic details, patients were examined for number of teeth according to Federation Dentaire Internationale system of tooth numbering.13 The study included examination of 28 teeth (3rd molars were excluded). The plaque score was evaluated by running a probe through four surfaces of the teeth (buccal, lingual, mesial and distal). Percentage of sites with presence of plaque was calculated according to the O’Leary Index.14 Probing, was performed at buccal, lingual, mesial and distal areas of the teeth, to record gingival bleeding according to the Ainamo and Bay’s gingival bleeding index.15 Clinical
attachment loss (CAL) was determined by examining periodontal pocket depth at 6 sites per tooth and level of recession via UNC (University of North Carolina)
periodontal probe.16 Periodontitis was classified as mild, moderate and advanced according to the degree of clinical attachment loss and number of sites affected.11 Intra and inter operator reliability was calculated at 95% and 90% respectively.
For evaluating glycemic levels in patients with periodontitis, gentle periodontal probing was performed at the site of periodontal inflammation and random gingival
crevicular blood glucose levels were recorded by a glucometers at the site of maximum bleeding. The patients having glycemic levels between 180-200mg/dl, were
classified as pre-diabetic, whereas, glycemic levels of more than 200mg/dl indicated diabetes. The prevalence of prediabetes and diabetes among chronic periodontitis patients was calculated as: Number of patients with pre-diabetes and diabetes/Total number of patients.
STATISTICAL ANALYSIS:
SPSS version 20 was used to carry out data analysis. Frequency and percentage was calculated for descriptive variables, whereas, mean and standard deviation was used for numerical data. Correlation of glycemic levels with age, number of teeth, gingival bleeding, plaque percentage and CAL was determined by Karl Pearson correlation coefficient formula. Multiple regression analysis was used to find the linear relationship of GCB glucose with periodontal disease parameters. Mean GCBG values in patients with mild, moderate and advanced periodontitis were evaluated by Analysis of variance (ANOVA) and post Hoc analysis.
RESULTS:
Out of 348 patients with chronic periodontitis, 42 percent were males, while 58 percent were females. The age range of the participants was 25 to 60 years. The age
of majority of participants (61.2%) was 40 years and above, with the mean age of 43+/-10.4 years. When gingival crevicular blood glucose levels were correlated with age of the patients, a correlation(r) of 0.403 was observed with a p value of <0.001(Table 2). The prevalence of pre-diabetes and diabetes was found to be 6.6% (23 out of 348 cases) and 14.3% (50 out of 348 cases).
The average number of teeth present among the participants was 25+/-3; with a minimum number of 20 and maximum number of 28 teeth (3rd molars were not included in the examination). When number of teeth present was correlated with gingival crevicular blood glucose levels, a negative correlation was observed (Table 2).
The average percentage of plaque containing surfaces was 74% with a minimum of 34% and maximum of 100%. When plaque percentage was correlated with gingival crevicular blood glucose levels, a weak correlation was observed. While, gingival bleeding and CAL showed a strong correlation with glycemic levels (Table 1).
Table 1: Correlation of Gingival crevicular blood glucose levels with age, number of teeth, plaque percentage, clinical attachment loss and bleeding on probing
 GCBG= Gingival crevicular blood glucose, CAL= Clinical attachment loss, BOP= Bleeding on probing, r= Pearson Correlation coefficient, p value= Level of Significance (taken at less than 0.05), N= Sample size
GCBG= Gingival crevicular blood glucose, CAL= Clinical attachment loss, BOP= Bleeding on probing, r= Pearson Correlation coefficient, p value= Level of Significance (taken at less than 0.05), N= Sample size
Multiple linear regression revealed significant linear association between periodontal parameters and GCB glucose value with r2 (coefficient of determination) of 0.633 at a level of significance of <0.001. Bleeding on probing and CAL were found to be significant predictors of gingival crevicular blood glucose levels, while age and plaque percentage revealed insignificant prediction values (Table 2).
Table 2: Multiple linear regression model for GCB as independent variable and periodontal disease parameters as independent variables
 Multiple regression model summary: r=0.796, r2= 0.633 (p<0.001). Beta= Beta coefficient -comparison of strength of effect of independent variable on dependent variable, t= t statistic, Sig= Level of significance (taken at 0.05)
Multiple regression model summary: r=0.796, r2= 0.633 (p<0.001). Beta= Beta coefficient -comparison of strength of effect of independent variable on dependent variable, t= t statistic, Sig= Level of significance (taken at 0.05)
Analysis of variance (ANOVA) was used to check the difference in mean of GCB glucose values between 3 groups according to severity of periodontitis. A significant difference in mean was observed between the groups of mild, moderate and advanced periodontitis (Table 3).
Table 3: ANOVA showing difference in mean GCBG levels between groups of mild, moderate and advanced periodontitis patients
 GCBG=Gingival Crevicular blood glucose, SD=Standard deviation, F= F-statistic (variation between group means/variation within group means), Sig= Level of significance (taken at 0.05)
GCBG=Gingival Crevicular blood glucose, SD=Standard deviation, F= F-statistic (variation between group means/variation within group means), Sig= Level of significance (taken at 0.05)
A significant difference in mean GCB glucose values between mild, moderate and advanced periodontitis groups was found when Post Hoc Tukey’s analysis was performed (Table 4).
Table 4: Post Hoc Tukey’s analysis showing difference in mean between the mild, moderate and advanced periodontitis groups
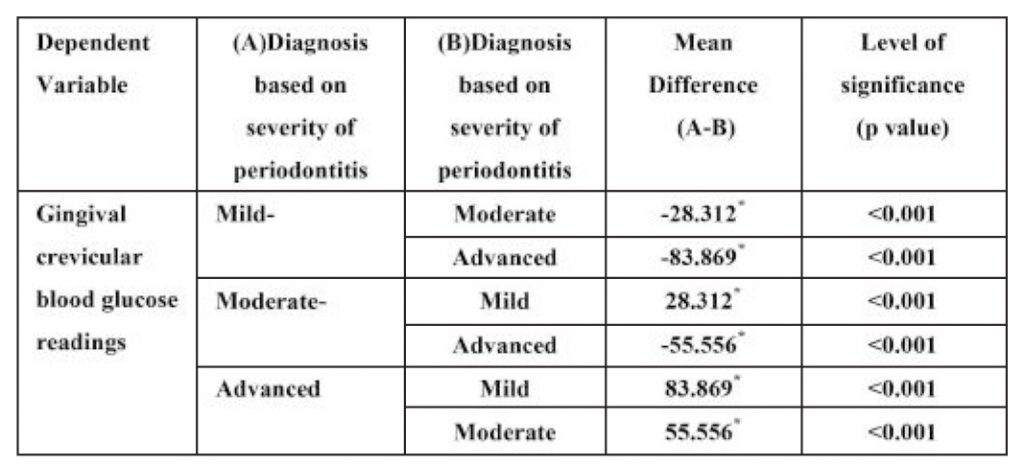 *Mean difference is significant if p value is less than 0.05
*Mean difference is significant if p value is less than 0.05
The mean plot visualizes the variability in GCB glucose values in mild, moderate and advanced periodontitis groups (Figure1).
Figure 1

diagnosis on the basic of severity of periodontitis
DISCUSSION:
Periodontitis has been known to affect about 20-50% of world’s population and has a high prevalence in developing countries, which makes it a public health concern.3 Literature suggests that there exists a strong association between periodontitis and diabetes.6,17-20 Patients with type 2 diabetes with chronic periodontitis, have 3.2 times increased mortality risk as compared to periodontally healthy individuals.3 Due to this strong association between both the diseases, it is necessary to screen blood glucose levels in periodontal patients. Therefore, in this study, we assessed GCBG (gingival crevicular blood glucose) levels via glucometers to screen chronic periodontitis patients for diabetes. According to a study carried out by Meo et al. in 2016, the prevalence of diabetes was recorded as 11.7% in Pakistan.21 Whereas, in our study, the prevalence of pre-diabetes and diabetes was found to be 21% (6.6% and 14.7%) in chronic periodontitis patients. Our study supports the concept that chronic periodontitis increases the chances of insulin resistance and promotes hyperglycemia, which is the major cause of
increased prevalence of diabetes in periodontal patients. Majority of patients included in our study were above 40 years of age. When age was correlated with gingival crevicular blood glucose levels, a moderate correlation of 0.403(r) at p value of <0.001 was observed. Based on this observation, our study suggests that glycemic levels are significantly associated with increase in age. The study by Ko et al. also reports that age and blood glucose levels are significantly correlated (r=0.114, p<0.001).22 Another study by Kalyani et al. reports that there is altered glucose metabolism with aging which leads to increased blood glucose levels.23
Dental plaque is an adherent film of microorganisms and food debris, found on the external surface of the teeth.24 In our study we found weak association between dental plaque and glycemic levels, as the plaque percentage at the dental visit depends on the personal dental hygiene of the patient and is not majorly affected by the blood glucose levels.
Gingival bleeding and clinical attachment loss are important clinical parameters of periodontitis.25 Gingival crevicular blood glucose levels demonstrated strong
correlation with bleeding on probing (r=0.760, p<0.001) and CAL(r=0.733, p<0.001) which indicates that hyperglycemia plays an important role in periodontal
inflammation and alveolar bone resorption. Our study also proves that CAL and gingival bleeding are significant predictors for glycemic levels. Alasqah et al., in their study, found similar results that CAL was significantly increased in patients with pre-diabetes and diabetes as compared to non-diabetic patients.26 The study by Oyapero et al. also support our findings.27 Kogawa et al. also reported in their study that CAL and gingival bleeding were significantly increased in patients with poorly controlled blood glucose values (p=0.05).28 The reason for increased gingival bleeding in diabetics could be an aggravated inflammatory response which develops due to high blood glucose levels in the body.6 A study by Sayeeganesh et al. also reported significant increase in gingival bleeding tendency in diabetics as
compared to non-diabetic individuals (p<0.01).29 In our study, when regression analysis was performed, periodontal parameters of bleeding on probing and clinical attachment loss where found to be significant risk indicators for increased GCBG levels (Table3), which proves that periodontitis increases the risk of hyperglycemia and leads to diabetes.
The studies conducted by Liccardo et al. and Gaurav et al. support our findings that periodontitis increases the risk of diabetes.30,31 Poor glycemic control in periodontitis leads to worsened gingival health and increase in inflammatory response, which causes increased gingival bleeding and bone resorption in periodontitis patients, leading to eventual loss of teeth. The total number of teeth showed significant negative correlation with glycemic levels, in our study,
which indicates that hyperglycemia has a significant association with tooth loss in chronic periodontitis patients (Table 2).
For evaluating the relationship of severity of periodontitis with glycemic levels, periodontitis was categorized into mild, moderate and advanced according to the criteria provided by Eke et al. and the mean GCB glucose levels of each group were compared.11 In our study, the patients with advanced periodontitis had the highest mean GCBG levels (198+/-78 mg/dl), while, the mild periodontitis patients showed the lowest GCBG values(111+/-28 mg/dl) .When the difference in mean of GCB glucose values was analyzed between the groups of patients having mild, moderate and advanced periodontitis, a highly significant difference was observed (F=65.125, p value <0.001). Post hoc Tukey’s analysis confirmed that significant difference in mean GCBG glucose was present between groups with increasing severity of periodontitis (Table 4). Through these findings, our study confirms the two-way relationship between glycemic levels and severity of clinical parameters of periodontitis and provides evidence that increase in glycemic levels increase in periodontal inflammation. The limitation of this study is that random gingival crevicular blood glucose samples were taken in our study on point and not compared with fasting blood glucose levels. Further studies are recommended to compare this screening method with conventionally used blood glucose screening procedures and for their association with periodontal disease parameters.
CONCLUSION:
Through this study we conclude that clinical periodontal disease parameters and severity of periodontitis are significantly correlated with gingival crevicular blood glucose levels.
CONFLICT OF INTEREST:
None
FUNDING:
The study was self-funded by the researcher
DISCLAIMER:
This manuscript is a component of a research study called “Clinicopathological correlation of disease severity in periodontitis with crevicular blood glucose estimation”
REFERENCES:
- Knen E, Gursoy M, Gursoy K. Periodontitis: A Multifaceted Disease of Tooth-Supporting Tissues. J Clin Med. 2019; 8:1135. https://doi.org/10.3390/jcm8081135
- Konkel JE, O’Boyle C, Krishnan S. Distal Consequences of oral inflammation. Front Immunol. 2019; 10:1403. https://doi.org/10.3389/fimmu.2019.01403
- Nazir MA. Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci. 2017; 11:72-80.
- Llambs F, Arias-Herrera S, Caffesse R. Relationship between diabetes and periodontal infection. World J Diabetes. 2015; 6:927-35. https://doi.org/10.4239/wjd.v6.i7.927
- Matthews DC. The relationship between diabetes and periodontal disease. J Can Dent Assoc. 2002; 68:161-164.
- Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, et al. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012; 55:21-31. https://doi.org/10.1007/s00125-011-2342-y
- Zizzi A, Tirabassi G, Aspriello SD, Piemontese M, Rubini C, Lucarini G. Gingival advanced glycation end-products in diabetes mellitusassociated chronic periodontitis: an immunehistochemical study. J Periodontal Res. 2012; 48:293-301. https://doi.org/10.1111/jre.12007
- Gurav AN. Periodontitis and insulin resistance: casual or causal relationship? Diabetes Metab J. 2012; 36:404-11. https://doi.org/10.4093/dmj.2012.36.6.404
- Altamash M, Klinge B, Engstrm PE. Periodontal treatment and HbA1c levels in subjects with diabetes mellitus. J Oral Rehabil. 2016; 43:31-8.
- https://doi.org/10.1111/joor.12339
- Pei XY, He L, Ouyang XY. Proposing a novel, three-level definition of periodontitis using probing depth, clinical attachment loss and bleeding on probing: Analysis of a rural Chinese population. Chin J Dent Res. 2017; 20:89-96. https://doi:10.3290/j.cjdr.a38273
- Eke PI, Dye BA, Wei L, Thornton-Evans GO, Genco RJ. Prevalence of periodontitis in adults in United States: 2009-2010. J Dent Res. 2012; 91:914-20. https://doi.org/10.1177/0022034512457373
- Bokhari SAH, Sohail AM, Imran MF. Periodontal disease status and associated risk factors in patients attending a dental teaching hospital in Rawalpindi, Pakistan. J Indian Soc. 2015; 19,678-82. https://doi.org/10.4103/0972-124X.156882
- Kannan D, Gurunathan D. Comparison of two systems of tooth numbering among undergraduate dental students. Indian J Dent Res. 2016; 27:378-82.
- https://doi.org/10.4103/0970-9290.191885
- O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J periodontal. 1972; 43:38. https://doi.org/10.1902/jop.1972.43.1.38
- Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975; 25:229-35.
- Deepa R, Prakash S. Accuracy of probing attachment levels using a new computerized cemento-enamel junction probe. J Indian Soc
- Periodontol. 2012; 16:74-9. https://doi.org/10.4103/0972-124X.94609
- Pontes C, Flyvbjerg A, Buschard K, Holmstrup P. Relationship between Periodontitis and Diabetes: Lessons from Rodent Studies. J
- Periodontol. 2007; 78:1264-75. https://doi.org/10.1902/jop.2007.060491
- Pathak AK, Shakya VK, Chandra A, Goel K. Association between diabetes mellitus and periodontal status in north Indian adults. Eur J
- Gen Dent. 2013; 2:58-61. https://doi.org/10.4103/2278-9626.106815
- Bascones-MartÃneza A, Muñoz-Corcuera M, Bascones-Ilundain J. Diabetes and periodontitis: A bidirectional relationship. Med Clin
- (Barc). 2015; 145:31-5. https://doi.org/10.1016/j.medcli.2014.07.019
- Kumar M, Mishra L, Mohanty R, Nayak R. Diabetes and gum disease: the diabolic duo. Diabetes Metab Syndr. 2014; 8:255-8. https://doi.org/10.1016/j.dsx.2014.09.022
- Meo SA, Zia I, Bukhari IA, Arain SA. Type 2 diabetes mellitus in Pakistan: Current prevalence and future forecast. J Pak Med Assoc. 2016; 66:1637-42.
- Ko GT, Wai HP, Tang JS. Effects of age on plasma glucose levels in non-diabetic Hong Kong Chinese. Croat Med J. 2006; 47:709-13.
- Kalyani RR, Egan JM. Diabetes and altered glucose metabolism with aging. Endocrinol Metab Clin North Am. 2013; 42:333-47. https://doi.org/10.1016/j.ecl.2013.02.010
- Seneviratne CJ, Zhang CF, Samaranayake LP. Dental plaque biofilm in oral health and disease. Chin J Dent Res. 2011; 14:87-94.
- Lang NP, Bartold PM. Periodontal Health. J Periodontol. 2018; 89:S9-S16. https://doi.org/10.1002/JPER.16-0517
- Alasqah M, Mokeem S, Alrahlah A, Al-Hamoudi N, Abduljabbar T, Akram Z. Periodontal parameters in prediabetes, type 2 diabetes mellitus, and non-diabetic patients. Braz Res. 2018; 32:e81.M https://doi.org/10.1590/1807-3107bor-2018.vol32.0081
- Afolabi O, Adetokunbo A, Oyinkansola S, Okeoghene A. Effect of glycemic control on periodontal disease and caries experience in diabetic patients: A pilot study. J Interdiscip Dent. 2019; 9:99-107. https://doi.org/10.4103/jid.jid_67_18
- Kogawa EM, Grisi CP, Falcão DP, Amorim A, Rezende B, Da Silva R. Impact of glycemic control on oral health status in type 2 diabetes individuals and its association with salivary and plasma levelsof chromogranin A. Arch Oral Biol. 2016; 62:10-9. https://doi.org/10.1016/j.archoralbio.2015.11.005
- Sayeeganesh N, Basker K, Manovijay B, Saranyan R, Shanmugasundaram N, Vijayakumar N. Relationship between gingival bleeding and blood glucose level: a case-control study. Int J Med Res Rev. 2015; 3:588-92. https://doi.org/10.17511/ijmrr.2015.i6.111
- Liccardo D, Cannavo A, Spagnuolo G, Ferrara N, Cittadini A, Rengo C. Periodontal disease: A risk factor for Diabetes and Cardiovascular Disease. Int J Mol Sci. 2019; 20:1414. https://doi.org/10.3390/ijms20061414
- Gurav A, Jadhav V. Periodontitis and risk of diabetes mellitus. J Diabetes. 2011; 3:21-8. https://doi.org/10.1111/j.1753-0407.2010.00098.x
- M.Phil. Trainee, Department of Oral Biology, Ziauddin College of Dentistry, Ziauddin University, Karachi, Pakistan.
- Associate Professor, Department of Orthodontics, Ziauddin College of Dentistry, Ziauddin University, Karachi, Pakistan
- Professor, Principal and Dean of Dental Sciences, Ziauddin College of Dentistry, Ziauddin University, Karachi.
- Assistant Professor, Department of Oral Biology, Ziauddin College of Dentistry, Ziauddin University, Karachi.
- Corresponding author: Dr. Quratulain Saeed < ainysaeed.aidm@gmail.com >

