Pamphlet or a Lecture, which Method is more Effective in Educating Children about Proper Ways of Tooth Brushing? Quasi-Experimental Study
OBJECTIVE: To compare the effect of educating proper tooth brushing techniques via lecture or pamphlet on the reduction of dental plaque score among 12-year-old schoolchildren from subset Karachi.
METHODOLOGY: A quasi-experimental study was performed from September to December 2021 in three underprivileged Karachi schools. After ethical approval schools were selected based on convenience sampling. Subjects were selected by random sampling and were divided into groups A, B, and C. The children of groups A&B (lecture& pamphlet) were taught tooth brushing as per American dental association criteria. The Plaque score at baseline was recorded. Group A was educated using a lecture with a live demonstration of brushing using models and charts. Group B was given Pamphlets, that had both text and illustrations, containing pictures of brushing techniques. Group C had no interventioni.e. a control group. The dental plaque score was calculated using the Loe and Silness scale. The Plaque score was measured at baseline (0), after one month, and after three months. RESULT: At baseline mean, the mean plaque score was 1.381±0.636, at 1-monthfollow-up 1.161±0.562, and at 3 months follow-up 1.065±0.658. There was a significant decline in mean plaque score in group A(lecture) followed by Group B(Pamphlet) after three months of intervention. No difference was seen in the control group.
CONCLUSION: The study concluded that health education programs promote oral hygiene among school-going children as a significant improvement in mean plaque score reported from baselines to 3 months follow-up.
KEYWORDS: Toothbrushing Technique, Dental Plaque, Lecture, intervention, Pamphlet.
HOW TO CITE: Amir HN, Zaidi AB, Mohiuddin S, Firdous SN. Pamphlet or a lecture, which method is more effective in educating children about proper ways of tooth brushing? quasi-experimental study. J Pak Dent Assoc 2023;32(4):114-119.
DOI: https://doi.org/10.25301/JPDA.324.114
Received: 28 September 2022, Accepted: 17 January 2024
INTRODUCTION:
Oral health is a key factor in overall health and the quality of one’s life. Oral diseases include dental caries, periodontal disease, oral cancer, oral symptoms of HIV, or-dental trauma, cleft lip and palate, and noma.1 Oral infections, such as dental caries and periodontal disease, has globally a destructive impact on oral health situation. Treatment of dental problems is likely to exceed the available resources in low-income countries.
Good dental health is an important element of sustaining a high quality of life.2
Oral diseases are on the rise in emerging countries owing to rapid changes in diet, nutrition, and lifestyles. Poor oral hygiene contributes to the formation of dental plaque, which has a significant impact on oral health. This is the precursor to dental caries and periodontal disease, which can lead to tooth loss if not treated appropriately.3
Dental plaque is considered the possible causative agent of major dental diseases such as caries and periodontal disease. An essential element in a preventive dental program is a well-organized plaque control program. The core of this preventive regimen including the mechanical and chemical plaque control measures is comprehensive home oral hygiene.4
The removal of dental plaque from the tooth surface is essential for the prevention of oral illnesses such as dental caries and periodontitis. As a result, disruption of plaque formation regularly is critical for reducing and controlling plaque-related oral illnesses.3 Assuming that toothbrushing is an important aspect of an effective plaque management program, good oral hygiene would be determined by the effectiveness of the specific method and the simplicity with which the procedure is performed.4
For plaque accumulation, tooth brushing is considered the simplest applicable mechanically preventive measure. Effective and regular plaque control measures ensure good periodontal as well as dental health.5-6
Poor oral hygiene results due to microbial plaque aggregation on the teeth and oral structure further damaging the tooth in form of dental caries, gingivitis, and periodontal disease.7 Effective plaque control not only depends on the toothbrush type but also on the proper toothbrushing technique.8
Schools are the ideal place to assess and teach children’s oral health knowledge and practice because this is when lifelong beliefs and critical abilities are formed. Teachers and parents have an essential role in improving children’s dental health. Regular, low-cost interventions such as school based health education have also been found to be effective in the short run.9
Although schools serve as a foundation for shaping children’s behavior, it is vital to improve their dental health habits through school dental health education.10 Overall positive and acceptable oral health behaviors can be achieved effectively with the support of school-based health education programs using simple and cost-effective strategy to reach and teach them.11 It has been claimed that instruction in tooth brushing techniques is particularly beneficial in improving oral hygiene and that dentists should also consider the patients’ physical dexterity.12
School management teams must take an active role in educating students and reviewing their oral health status regularly. It is important to emphasize how dental health can affect overall health and how oral health measures can aid in the prevention of systemic disorders. To create a solid and supportive structure surrounding the children, regular feedback from parents to instructors and vice versa is required. The key to the future’s overall development is to educate the children.13 Oral illnesses should be avoided before they arise, and simple oral hygiene procedures like brushing and flossing every day will help.2 Short-term oral health initiatives and health education can enhance oral hygiene and boost children’s health. Coordination efforts between school personnel, parents, and health specialists should be increased to produce long-term benefits.14
A previous study reported that educational intervention involve four meetings about oral hygiene in which the researcher educates the students about the prevention of diseases which are caused by poor oral hygiene, and appropriate way of tooth brushing had led to the improvement in dental/oral health.15 The improvement by educational intervention and by proper techniques of tooth brushing was seen among school going children.7,14,15,16
There is a scarcity of data regarding interventional methods to assess oral hygiene of school children therefore, this current study will be fruitful in assessing the effect of proper tooth brushing techniques that will be taught via lectures and pamphlets among school children for the reduction of dental plaque. Therefore, the objective of the current study was to compare the effect of educating proper tooth brushing techniques via lecture or pamphlet on the reduction of dental plaque scores among 12-year-old schoolchildren from subset Karachi.
METHODOLOGY:
The Quasi-experimental study was conducted for 4 months from September to December 2021. The study was conducted after approval from the ethical review committee of Altamash Institute of Dental Medicine (AIDM) Karachi. The sample size of n=42 per group was estimated by using the WHO calculator for sample size calculator by keeping a 95% confidence level. The mean plaque index (PI) for educating proper brushing techniques via lecture was 0.89 with a standard deviation of 0.40 as suggested by (Javad Ramezaninia et al,.2018).7 The level of significance was 0.05, power of the test was 80%. Added 20% attrition rate or loss to follow-up n=42 per group was 50.4 rounded off to n=56. For the selection of study subjects, sixth-grade students were approached and screened for inclusion and exclusion criteria and they were selected by a simple random sampling method. The Principal investigator used the lottery method to select 56 chits and the selected study subjects were later enrolled in the study. On the paper chit, students’ class roll numbers were listed. All study subjects from three schools were chosen using the simple random sampling selection approach and three groups A, B, and C were formed, one from each school. Group A and B were interventional or experimental groups and Group C was the control group. After school selection is written permission from each school administration was taken.
The main data collection tools werethe oral examination kit, performa,and,Silness and Loeplaqueindex, a performa was filled by the investigator containing data like age, gender,socioeconomic status, and parents’ education. The Plaque score at baseline (T0) was recorded. After the baseline assessment, the study subjects of the Group A&B (lecture & pamphlet) were taught the Bass tooth brushing technique as per American dental association criteria (Place your toothbrush at a 45-degree angle on your gums then gently move it back and forth, brush outer inner and chewing surfaces of your teeth). Both groups Group A was educated using a lecture for about 10 minutes with a live demonstration of brushing using models and charts, both were taught in English and Urdu. Group B was given Pamphlets, that had both text and illustrations, containing pictures of brushing techniques. Group C had no intervention. The plaque scores were assessed after one month (T1) and three months (T2) from the baseline assessment.
The data was entered in SPSS version 22.0 mean and SD was calculated for quantitative variables. The normality of the data was checked via the Shapiro-Wilk test. The data was non-parametric therefore Kruskal Wallis test was applied.Friedman test was used for the analysis of multiple observations i.ebaseline,1 month 3-month, and among all 3 groups. For further sub-group analysis,Wilcoxon signed rank test was used. The level of significance was p <0.05.
RESULTS:
Table1 showed the frequency distribution of Plaque scores at different visits and it was seen that out of a total of 168 study participants 91(54.2%) had 0.1-0.9 mm,63(37.5%) had 1-1.9mm and only 9(5.4%) had 0mm Plaque score at baseline (T0). At one month of follow-up (T1), 117(69.6%) had a plaque score of 0.1-0.9 mm whereas

13(8%) had a 0 mm plaque score this value is 3% greater compared to the Baseline. At three-month follow-up (T2)101(60.1%) had a plaque score 0-1 and 29(17.3%) had a plaque score of 0mm hence this value is 12% greater compared to baseline (5.4%). Moreover, at baseline 5(3%) had a plaque score of 2-3mm whereas after three months follow up it decreased to 2(1.2%).
Table 2 shows Mean±SD of Plaque Score among Group A, B, and C, and a statistically significant decline in mean plaque score was reported only in Group A (lecture) from 1.48±0.603 to 0.732±0.486 followed by Group B (Pamphlet) 1±0.572 to 0.88±0.541after three months of intervention. 1.66±0.549 to 1.60±0.596 shows that no difference was seen

in the control group.The Wilcoxon signed-rank test for further analysis shows a statistically significant difference (p-value <0.05) among all the observations recorded in the lecture group.
Table 3 shows a Pairwise comparison of plaque scores among study groups and it was seen that for baseline plaque scores there is statistically a significant difference between Group A(Lecture) and Group B (Pamphlet) as well as between-group B (Pamphlet) and Group C (Control) showing p-value <0.05 each, whereas no significant difference between Group A (Lecture) and group C (Control) was found (p=0.312)
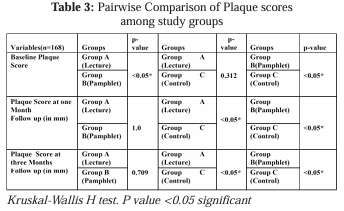
For the Plaque score at one month follow up there is statistically a significant difference between Group A (Lecture) and Group C (Control) as well as for group B (Pamphlet) and Group C (Control) showing p=<0.05 each. Furthermore, no statistically significant difference between Group A (Lecture) and B (Pamphlet) was seen (p=1.0).
For Plaque score at three months follow up a statistically significant difference between Group A (Lecture) and Group C (Control) as well as for group B (Pamphlet) and Group C (Control) was found; showing a p-value <0.05 each whereas no statistically significant difference between Group A (Lecture) and B (Pamphlet) was reported (p=0.709)
DISCUSSION:
This study found that a school-based, simple-to-organize, low-cost educational intervention can help 12-year-old students improve their oral hygiene. The individuals were picked at random and had similar background characteristics, such as similar age ranges and socioeconomic positions, as well as being from the same city school areas. The effectiveness of a dental health program was investigated in this study, and it was discovered that children who received the program had much lower mean Plaque index scores. Any combination of learning experiences aimed at encouraging behaviors that are better for one’s well-being is referred to as health education. People, families, organizations, and communities may be responsible for these actions or behaviors. As a result, health education may encompass educational initiatives for all people. Correct information or understanding about health does not always lead to optimal health behavior, as has been documented in dentistry and other professions. Nonetheless, the knowledge could be used to provide correct information about health and healthcare technologies to populations, allowing people to take action to protect their health. The main goal of intervention strategies is to shift personal behavior from health-harming to health-promoting.14 This has traditionally been accomplished through the provision of information, education, and counseling.17 Overall health promotion is vital, but oral health promotion is the most significant; it primarily aims to prevent mouth illness through health education. Oral health care should be provided to all children, not just those in primary school. Many forms of health education programs are planned to enhance the oral health status of children and to create good oral health knowledge, attitude, attitudes, and healthy behaviors. In available literature, it is stated that tooth brushing, food, nutrition activities, and dental flossing are all part of oral health education.17 The goal of oral care education and well-designed interventions is to raise schoolchildren’s awareness of oral health, which can lead to changes in oral health behavior and improved oral health. Oral health and everyday oral hygiene are intertwined, and neglecting oral hygiene leads to diseases such as dental caries, gingivitis, and a variety of others. On the other hand, numerous lifestyle choices such as eating too much, consuming sugary drinks, smoking cigarettes, and drinking alcohol have an impact on oral health, however oral health promotion techniques are promoting preventive intervention. As a result, it is possible to control all of these behaviors in school settings to improve the physical environment and provide oral health education through school policy.15
Similar to our study a previous study by Javad Ramanzania et al, in 2018 also reported the same findings at two months follow-up. In their study, a decline in PI was reported in the lecture group followed by the Pamphlet group.7 Dental/Oral health education results in improvement of oral hygiene in the school settings in which different methods were implemented.16 However, while different dental/oral health education approaches were compared, Yazdani et al,. found leaflets method more successful than videotapes and that a culturally relevant film showed an improvement in oral hygiene among Nigerian youngsters.18
Writing, audio-visual, and spoken methods are the three basic types of learning approaches.7 The authors employed a pamphlet and a lecture as two of the three main modalities of dental/oral health education. The pamphlet, could not adequately convey the content and the intricacies of practical instruction. Verbal education/Lectures using a dental model required fewer specialist equipment and facilities and allowed youngsters to see how to brush more carefully. The lecture approach is advantageous since it allows many students to learn at the same time. The lecture technique is simple to use, convenient, and widely adopted, with a specified teaching plan, location, time, and flexibility.19 Contradictory findings in plaque index were observed by Cehyan D et al., from baseline.11 Education with regular proper brushing adoption proved significant for reducing plaque accumulation for preschool children from baseline to 1st and 2nd follow up visits but later at 6th month follow up it matches baseline, hence Plaque index again rises.11
Our study found that out of a total of 168 study participants only 9(5.4%) had a 0mm Plaque score at the start of the study. Later at one month of follow-up after baseline 13(8%) had a 0 mm plaque score this value is 3% greater compared to the baseline score. Moreover, at three months follow up after baseline 29(17.3%) had a plaque score of 0m hence this value is 12% greater compared to baseline (5.4%). At baseline 5(3%) had a plaque score of 2-3mm whereas after three months follow up it decreased to 2(1.2%). Alike our study a reduction in stage 1 plaque was reported from 75.5 % to 66.5% post-intervention.20 Another study found that the experimental group’s overall oral hygiene showed a 54.58% improvement, while the control group showed no improvement. Compared to the control group(4.56%) the mean plaque score was improved by 57.67% in experimental group.21 After six months, there was a pattern for the control group to brush less frequently and accumulate more dental plaque. Compared to the control group, the intervention group’s members showed better oral health knowledge, behaviour, and hygiene. A single school-based programme for oral health education can help 12-year-old students learn more about oral health and stop their short-term hygiene and behaviour from declining.22 The reason for the similarity between our study and previous literature could be the same age group 12 years old encountered in both national and international studies.7,14,15,16,20,21,22 Another study observed reduction in plaque accumulation in both the 9-year student and teacher groups. It was discovered that both OHE programmes improved oral health and plaque control knowledge and behavior irrespective of age differences among group. Moreover similarities of social and cultural norms prevailing in the society may lead to a better understanding of oral health education.23 Programs in schools that promote oral health have shown promising results, particularly when they involve parents, teachers, and students.24 School-based interventions can be effective in reducing the burden of oral disease among primary school children. Further research is required to provide evidence of effectiveness of primary school-based interventions to improve oral health.25
The limitation of the study was the lack of parents and teachers with selected subjects as they both also play an important part in oral health promotion and the development of habits among children. Secondly, the researcher used a combination method of education i.e. lecture along with demonstration therefore, we are not sure that the change in dental plaque scores was due to which educational activity. Thirdly, we have not seen any improvements in the pamphlets group, the reason might be lack of motivation to study them at home though we had given them to the subjects so they can take them to their home.
It is recommended that schools and institutes should encourage health promotion strategies such as behavior change approaches in early childhood by incorporating oral health messages in the school curriculum and teachers do emphasize to school children about tooth brushing twice a day every day. Also, to check oral hygiene as a part of their dental checkup once in six months.
CONCLUSION:
Our study concluded that a significant reduction in meanplaque score was recorded from baseline to one month and three months follow-up in the lecture group. Oral hygiene instructions through lecture was an effective strategy for reducing plaque sores. However, the pamphlet group did not show any significant improvement in plaque scores.
ETHICS APPROVAL:
Ethical approval was obtained before study initiation by the institutional review board (Ref#AIDM/RDR/10/2021/03). All procedures performed in studies involving human participants were in accordance with the ethical standards of the Helsinki declaration.
DISCLAIMER:
None
CONFLICT OF INTEREST:
None
SOURCE OF FUNDING:
None
REFERENCES:
1. World Health Organization. Fact sheet: Oral health, 2020. Accessed on 10 July 2020.’
2. Al-Tayar BA, Ahmad A, Sinor MZ, Harun MH. Oral health knowledge, attitude, and practices among Yemeni school students. J Int Oral Health. 2019;11:15. https://doi.org/10.4103/jioh.jioh_176_18
3. Reddy, M.P., Lakshmi, S.V., Kulkarni, S., Doshi, D., Reddy, B.S. and Shaheen, S.S., 2016. Impact of oral health education on plaque scores with and without periodic reinforcement among 12-year-old school children. J Ind Assoc Public Health Dent. 14, p.116.
https://doi.org/10.4103/2319-5932.183806
4. Ilyas, M., Ashraf, S. and Jamil, H., 2018. tooth brushing techniques: relative efficacy and comparison in the reduction of plaque score in 8 11 years old children. Professional Med J, 25, pp.135-139.
https://doi.org/10.29309/TPMJ/2018.25.01.552
5. Ceyhan D, Akdik C, Kirzioglu Z. An educational programme designed for the evaluation of effectiveness of two tooth brushing techniques in preschool children. Eur J Paediatric Dent. 2018;19:181-6.
6. Raviteja NV, Prasad MG, Radhakrishna AN, Saujanya K, Kumar KS, Divya DV, Sundeep RV. evaluation of mechanical plaque removal effectiveness oftoothbrush and its modifications in intellectually disabled children.
7. Ramezaninia J, Naghibi Sistani MM, Ahangari Z, Gholinia H, Jahanian I, Gharekhani S. Comparison of the effect of toothbrushing education via video, lecture and pamphlet on the dental plaque index of 12-year-old children. Children. 2018;5:50.
https://doi.org/10.3390/children5040050
8. Hayasaki H, Saitoh I, Nakakura-Ohshima K, Hanasaki M, Nogami Y, Nakajima T, Inada E, Iwasaki T, Iwase Y, Sawami T, Kawasaki K. Tooth brushing for oral prophylaxis. Japanese Dent Sci Review. 2014;50:69-77.
https://doi.org/10.1016/j.jdsr.2014.04.001
9. Kanagavelu AS, Chandran A, Brinda J. Oral hygiene practices and knowledge among children of age 10-13 years in a private school in Chennai, South India. Int J Community Med Public Health. 2020;7:4093.
https://doi.org/10.18203/2394-6040.ijcmph20204382
10. Reddy MP, Lakshmi SV, Kulkarni S, Doshi D, Reddy BS, Shaheen SS. Impact of oral health education on plaque scores with and without periodic reinforcement among 12-year-old school children. J Ind Assoc Public Health Dent. 2016;14:116.
https://doi.org/10.4103/2319-5932.183806
11. Ceyhan D, Akdik C, Kirzioglu Z. An educational programme designed for the evaluation of effectiveness of two tooth brushing techniques in preschool children. Eur J Paediatric Dent. 2018;19:181 6.
12. Hebbal M, Ankola AV. Development of a new technique (ATP) for training visually impaired children in oral hygiene maintenance. Eur Archives of Paediatric Dent. 2012;13:244-7.
https://doi.org/10.1007/BF03262878
13. Kanagavelu AS, Chandran A, Brinda J. Oral hygiene practices and knowledge among children of age 10-13 years in a private school in Chennai, South India. International J Community Med Public Health. 2020;7:4093.
https://doi.org/10.18203/2394-6040.ijcmph20204382
14. Rana BK, Rizwan Z, Rizwan G, Zia H, Afzaal M, Tariq R. Integrated school-based child oral health education-An intervention with an impact. J Med Res. 2021;7:83-8.
https://doi.org/10.31254/jmr.2021.7305
15. Ahmad M, Hussain M, Afzal M, Gilani SA. Effectiveness of Health Education to Improve Oral Care of Primary School Children in a Rural Community of Pakistan. EC Dent Sci. 2019;18:01-9.
16. Demiriz L, Dede FO, Balli U. Impact of three different education methods on oral hygiene and theoretical knowledge of schoolchildren. Pesquisa Brasileiraem Odontopediatria e ClinicaIntegrada. 2018;18:3897.
https://doi.org/10.4034/PBOCI.2018.181.29
17. Jürgensen N, Petersen PE. Promoting oral health of children through schools-Results from a WHO global survey 2012. Community Dent Health. 2013 Dec 1;30(4):204-18.
18. Yazdani, R., Vehkalahti, M.M., Nouri, M. and Murtomaa, H. School based education to improve oral cleanliness and gingival health in adolescents in Tehran, Iran. Int J Paediatric Dent. 2009;19:274-281
https://doi.org/10.1111/j.1365-263X.2009.00972.x
19. Habib, E., Shiraz, A.S., Naseri-Kouzehgarani, G., Hooman, S. and Reza, M.M. The determinants of high school students smoking habits with special focus on teachers smoking in Iran: a population based study. Pneumologia (Bucharest, Romania), 2012; 61:28-33
20. Raj S, Goel S, Sharma VL, Goel NK. Short-term impact of oral hygiene training package to Anganwadi workers on improving oral hygiene of preschool children in North Indian City. BMC Oral health. 2013;13:1-7.
https://doi.org/10.1186/1472-6831-13-67
21. Subedi K, Shrestha A, Bhagat T, Baral D. Effectiveness of oral health education intervention among 12-15-year-old school children in Dharan, Nepal: a randomized controlled trial. BMC Oral Health. 2021;21:1-1.
https://doi.org/10.1186/s12903-021-01877-6
22. Nguyen VT, Zaitsu T, Oshiro A, Tran TT, Nguyen YH, Kawaguchi Y, Aida J. Impact of school-based oral health education on Vietnamese adolescents: a 6-month study. International journal of environmental Res Public Health. 2021;18:2715.
https://doi.org/10.3390/ijerph18052715
23. Eden E, Akyildiz M, Sönmez I. Comparison of two school-based oral health education programs in 9-year-old children. Int Quarterly of Community Health Educ. 2019;39:189-96.
https://doi.org/10.1177/0272684X18819980

