Revisiting the Role of Periodontal Plastic Surgery in Regenerative Therapies Clinical Criteria and Biological Principles
One of the manifestations of periodontitis is bone loss and tooth mobility. Thus, periodontal regeneration plays a vital in reinstating the lost alveolar bone and periodontal tissue. This study aims at the different literary resource that highlight the role of periodontal plastic surgery; clinical criteria and biological principles that facilitates the process of regeneration. Several corrective steps are implemented for the management of chronic periodontal disease, such as the first line of intervention which is the non-surgical treatment that consists of Oral hygiene instructions and removal of biofilms. After non-surgical phase of treatment once the tissue is healed, surgical techniques are to be considered for the management of the remaining pockets also known as residual pockets or to formulate a gingival apparatus that promotes plaque control. However, if there is a loss of tissue it is quintessential to take into consideration regenerative procedures.
KEYWORDS: Periodontal plastic surgery, biological principals, regeneration
HOW TO CITE: Zia MH. Revisiting the role of periodontal plastic surgery in regenerative therapies clinical criteria and biological principles. J Pak Dent Assoc 2023;32(1):22-26.
DOI: https://doi.org/10.25301/JPDA.321.22
Received: 02 August 2022, Accepted: 01 April 2023
INTRODUCTION:
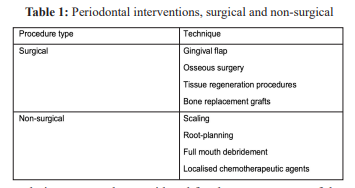
The purpose of periodontal regeneration is to rehabilitate the loss of supporting structures surrounding the tooth other than injury or periodontal disease. (Villar and Cochran, 2010).1 Several corrective steps are implemented for the management of chronic periodontal disease, such as the first line of intervention which is the non-surgical treatment that consists of oral hygiene instructions and removal of biofilms. (Reynolds et al., 20102
: Table 1). After nonsurgical phase of treatment once the tissue is healed, surgical
techniques are to be considered for the management of the remaining pockets also known as residual pockets or to formulate a gingival apparatus that promotes plaque control. (Koop et al., 2002).3 However, if there is a loss of tissue it is quintessential to take into consideration regenerative procedures. (Rojas et al., 2019).4 Illustrated in Fig 15 ; regeneration is a multifactorial approach which need several steps such as appropriate patient selection based on the potentiality of wounding healing, also the extent of the periodontal tissue loss and the influence of the nonsurgical regenerative methods. ( Rojas et al.,2019).4

Fig 1: Influental factors in periodontal regeneration. This figure illustrates the needs to control disease and consider a range of factors associated with inflammation and biofilm formation in order to justify regenerative approaches in periodontal surg
CLINICAL STANDARD FOR SURGICAL AND REGENERATIVE THERAPY:
Periodontal plastic surgery may be incorporated to facilitate wound healing as it can provide a conductive environment for the healing process. A variety of factors influence whether periodontal plastic surgery is appropriate for an individual patient, including their condition and whether specific surgical approaches are necessary. (Villar and Cochran,2010).1 It is to be understood that periodontal plastic surgical techniques to regenerate are divergent in context thus they consist of a variety of techniques, resulting in a general lack of consensus over the ideal or the best possible strategy and a wide range of factors contribute to this lack of consensus and one of them is patient suitability. (Tatakis et al., 2015).6 This argument has also put forward a debate that has been held responsible for the use of specific regenerative therapies, including guided tissue regeneration (GTR) and enamel matrix derivatives, both of which may have specific applicationsdepending on the clinical context in which they are applied (Rojas et al., 2019).4 Nevertheless, at the forefront remains an early and safe wound closure that leads to a successful regeneration. However, the integrity of wound closure is dependent upon the stability of the wound in the first postoperative week. Facilitated by the use the use of biomodulators that are the guided tissue regeneration and Enamel Matrix derived protein for primary intention healing. (Rojas et al., 2019).4 Although to advocate the practice of surgical approaches, in all forms of regenerative therapy, there is no well-defined and consistent clinical criteria. However, the results of several studies indicate that patient with specific characteristics may be subservient to surgical approaches. (Walter et al.,2011; Rojas et., 2019).7
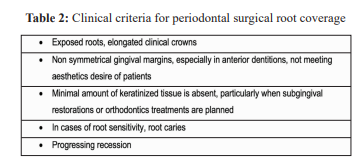
The above-mentioned specific characteristics are elimination of toxins from the root surface, space maintenance to facilitate movement of cells from intact periodontal ligament, wound stabilisation, and primary healing due to passive adaptation of the flap and complete wound closure (Hagi et al., 2014).8 To promote regeneration at times the surgical intervention may require augmentative materials. A non-resorbable membrane is the best possible example of augmentative material as tend to stabilize the site and promote wound healing. (Tatakis et al., 2015).6
SURGICAL METHODS FOR REGENERATIVE THERAPY:
In regenerative periodontal therapy the surgical methods implemented may vary. Thus, resulting in complexity in patient selection along with the indication for specific procedures. However, most surgical approaches evolve in concert with the formulation of flaps to encourage healing and to amplify local tissue (Rojas et al., 2019).4 Immobilized flaps or sedentary flaps also known as passive flaps can be advantageous for wound healing when regenerative bone procedures are performed, however, importance must be given to stability at the site of primary closure and not to allow tension to be introduced across the wound (Ronda and Stacchi,.2011).9 As if the flaps are to be unstable it may result in premature exposure of the augmented site Ronda and Stacchi, 2011).9 Overall, the dynamics of the flaps should be maintained throughout the regenerative procedure.
An analysis carried by Cortellini et al., 201710; In which they studied the patient outcomes and cost related to the applicability of the modified papilla preservation flaps, access flaps with membrane use and access flaps alone to illustrata long-term effect of regenerative approaches. Resulted in regenerative approaches (modified papilla preservation and access flaps with membrane) superseding the access flaps alone when it comes to long term outcomes. The use of the formal facilitates wound healing and tissue regeneration. Additionally, in the same study it was also illustrated that with the help of regenerative approaches the periodontal inflammation subsided and there was a minimal tooth loss. However, the cost associated with the regenerative approaches were higher. Concurrently, Nickles et al., 2017.11 In their retrospective case series also demonstrated that the implementation of periodontal regenerative approaches hampers an improved root coverage. Overall, considering the above-mentioned studies sufficient evidence can be drawn to support the role of regenerative approaches in patient with infraboney defects. However, it should be noted that these studies had some heterogeneity in patient analysis in lieu of the size and site of wound, therefore a tailored approach can also be an important aspect for care planning.
In periodontal plastic surgery a common technique used for regeneration is the use of coronally advanced flap (Nickkles et al., 2017).11 As it is found to be in high probability in cases of patients having gingival recession and are in dire need of root coverage either alone with the support of coronally advance flap or with the use of connective tissue graft underneath the flap (Cairo et al., 2016).12 However, it must be considered that in cases of root coverage the underlined thickness of the keratinized tissue is of significance as the interplay of the keratinized tissue resulted in esthetical
appealing results and determines the need of connective graft in addition to the coronally advanced flap alone. The use of coronally advance flap has also shown to reduces the surgical time, morbidity related to graft harvesting and maintaining a stable clinical outcome (Cortellini and pini prato.,2012).13
Overall, the leading strategy for periodontal plastic
surgery remains the use of coronally advance flap (Tatakis et al.,2015).6In clinical scenarios where there is a deep lingual recession and a lack of keratinized tissue the connective tissue graft wall method has been illustrated. (Zucchelli et al., 2016).14 This method incorporates placement of a connective tissue graft underneath a coronally advance flap, imparting a shape of gentle tissue wall. (Zucchelli et al., 2016).15 Evaluation of this method in exercise has in large part been restricted to case research or series (Gonzalez et al., 2015; Zucchelli et al., 2016; Zucchelli et al., 2017).15,16,17 even though proof shows that this method might also additionally promote root coverage and upgrades the volume/thickness of keratinised tissue. Further research might be required to triumph over the restrictions of case study.
FACTORS INFLUENCING SURGICAL OUTCOMES:
The selection of the surgical technique, anatomical factors and biological/physiological factors has an influence in the surgical outcome of periodontal plastic surgery (Nickles et al., 2017).11 Some of factors are depicted in
Fig 2.

Fig 2: Patient-related factors that influence regenaertive periodontal therapy outcomes. A range of factors can influence the sucess of periodontal techniiques during regenerative therapy, including local, systematic and behavioural factors. Bop, bleeding on probing; FMPS, full-mouth plague score. Adapted from Hagi et al., (2014: 188) 8 The healing pathology in periodontal plastic surgery or any periodontal therapy is influenced by the treatment of infections and control of systematic disease (e.g. diabetes). Thus, it is of significance to consider these factors before initiating therapy (Hagi et al.,2014).8 Evidence also points out towards sufficiency of the local blood supply next to the graft bed, attributes of the graft (size, characteristics of the border and thickness) parafunctional habits of patient such as smoking. (Camargo et al.,2001; Shkreta et al.,2018).18,19 Structural integrity of the defect is also a factor that influence the surgical outcomes. An intraosseous defect having a depth of more than 3mm with defect angle of less than 25 degrees results in greater potential of regeneration in contrast to shallower defect. Also, the number of the remaining walls surrounding the defects play a vital role. A defect with high number of remaining walls also called a contained defect is more likely to have an optimal heal (Hagi et al., 2014).8
A successful wound healing is dependent on vascularity of the surgical site. As immunological response and blood clotting is triggered by an adequate blood supply (Sculean et al.,2015).20 Certain areas such as root surface where is a scarcity of vascularity, alternative technique is implemented. Such as the use of scaffold formation in which matrix of growth factors and stem cells are held responsible for wound healing and repair (Lin et al.,2009).21 It is of clinical significance that the scaffold design should be sufficient for the cells to carry out adhesion/attachment and proliferation. However, challenges may arise in compromised soft tissues or areas of poor vascularity for the clot to form. Thus, rehabilitation is carried out by the support of platelet rich fibrin membranes. (Jankovic et al., 2012).22 Which provides an ideal environment for the blood clot to adhere resulting in wound healing and closure. It must be noted that systematic factors related to the patient are of paramount for the clotting factor to provide an optimal result.
Failure of periodontal regeneration is common among smokers. Literary resources (Silva et al.,2010)23 illustrated that excessive smoking that is 10 cigarettes per day downgrade
the success rate of periodontal regeneration because it effects  the blood supply and immunological activity during healing.
Additionally, it also minimizes the risk of infection resulting in a stable post-surgical environment to ease the process of wound healing. Usually, wounds that are in context with periodontal surgery are sensitive in nature as the tooth structure projection hamper bacterial contamination of the wound. (Susin et al., 2015).24
To guarantee the effectiveness of regenerative treatments, firstly it is of significance to identify patients who are suitable for surgery. This consist of pre-surgical protocol that ensures in reducing the risk of infection and compromised healing. Secondly, selection of the appropriate surgical techniques based on the clinical scenario, and lastly, maintaining optimal post-surgical care. (Rojas et al., 2019).4
In aspect to uncontained defects, with limited number of adjacent osseous wall present variation in the surgical approach is justified. In such cases crestal incision is preferred. However, there is a general scarcity of consensus in the evidence comparing the effectiveness of different techniques and approaches, therefore clinician should opt for the

CONCLUSION:
There is no doubt now that when it comes to optimal regeneration in patient with chronic periodontal disease and loss of tissue, periodontal plastic surgery remains at the forefront. However, as a clinician it is important to carry out a comprehensive assessment of patient health, variables associated with wound size and shape. Also, the risk factors that can result in compromised wound healing because all  these factors will affect the choice of surgical approach and the precise nature of the technique. Whereas to improve results, patient behaviour and parts of surgical methods should be targeted. Still more research is needed to assess alternative regeneration techniques in conjunction with periodontal plastic surgery, taking both clinical and cosmetic outcomes into account.
CONFLICT OF INTEREST
None declared
REFERENCES
- Villar, C. C., & Cochran, D. L. (2010). Regeneration of periodontal tissues: guided tissue regeneration. Dent Clin, 54:73-92. https://doi.org/10.1016/j.cden.2009.08.011
- Reynolds, M. A., Aichelmann-Reidy, M. E., & Branch-Mays, G.L. (2010). Regeneration of periodontal tissue: bone replacement grafts. Dent Clin, 54;55-71. https://doi.org/10.1016/j.cden.2009.09.003
- Koop, R., Merheb, J., & Quirynen, M. (2012). Periodontalregeneration with enamel matrix derivative in reconstructive periodontal therapy: a systematic review. J Periodontol. 83:707-20 https://doi.org/10.1902/jop.2011.110266
- Rojas, M. A., Marini, L., Pilloni, A., & Sahrmann, P. (2019). Early wound healing outcomes after regenerative periodontal surgery with enamel matrix derivatives or guided tissue regeneration: a systematic review. BMC Oral Health. 19:76-86 https://doi.org/10.1186/s12903-019-0766-9
- Larsson, L., Decker, A. M., Nibali, L., Pilipchuk, S. P., Berglundh,T., & Giannobile, W. V. (2016). Regenerative medicine for periodontal and peri-implant diseases. J Dent Res. 95;255-266. https://doi.org/10.1177/0022034515618887
- Tatakis, D. N., Chambrone, L., Allen, E. P., Langer, B., McGuire,M. K., Richardson, C. R., & Zadeh, H. H. (2015). Periodontal soft tissue root coverage procedures: A consensus report from the AAP Regeneration Workshop. J Periodontol. 86: S52-S55. https://doi.org/10.1902/jop.2015.140376
- Walter, C., Weiger, R., & Zitzmann, N. U. (2011). Periodontal surgery in furcation-involved maxillary molars revisited-an introduction of guidelines for comprehensive treatment. Clin Oral Investi.15;9-20.
- Hagi, T. T., Laugisch, O., Ivanovic, A., & Sculean, A. (2014).Regenerative periodontal therapy. Quintessence Int. 45;185-92.
- Ronda, M., & Stacchi, C. (2011). Management of a coronally advanced lingual flap in regenerative osseous surgery: a case series introducing a novel technique. Int J Period Rest Dent. 31, 505-15
- Cortellini, P., Buti, J., Pini Prato, G., & Tonetti, M. S. (2017). Periodontal regeneration compared with access flap surgery in human intra-bony defects 20-year follow-up of a randomized clinical trial: tooth retention, periodontitis recurrence and costs. J Clin Periodontol, 44;1-10 https://doi.org/10.1111/jcpe.12638
- Nickles, K., Dannewitz, B., Gallenbach, K., Ramich, T., Scharf, S., Röllke, L., & Eickholz, P. (2017). Long-term stability after regenerative treatment of infrabony defects: A retrospective case series. J Periodontol. 88;536-542. https://doi.org/10.1902/jop.2017.160704
- Cairo, F., Cortellini, P., Pilloni, A., Nieri, M., Cincinelli, S., Amunni, F., & Tonetti, M. S. (2016). Clinical efficacy of coronally advanced flap with or without connective tissue graft for the treatment of multiple adjacent gingival recessions in the aesthetic area: a randomized controlled clinical trial. J Clin Periodontol. 43;849-856. https://doi.org/10.1111/jcpe.12590
- Cortellini, P., & Pini Prato, G. (2012). Coronally advanced flap and combination therapy for root coverage. Clinical strategies based on scientific evidence and clinical experience. Periodontol 2000. 59;158-184. https://doi.org/10.1111/j.1600-0757.2011.00434.x
- Zucchelli, G., Bentivogli, V., Ganz, S., Bellone, P., & Mazzotti, C. (2016). The connective tissue graft wall technique to improve root coverage and clinical attachment levels in lingual gingival defects. Int J Esth Dent. 11;538-48.
- Zucchelli, G., Mounssif, I., Marzadori, M., Mazzotti, C., Felice, P., & Stefanini, M. (2017). Connective Tissue Graft Wall Technique and Enamel Matrix Derivative for the Treatment of Infrabony Defects. Int J Period Rest Dent. 37;1-10 https://doi.org/10.11607/prd.3083
- Gonzalez, D., Cabello, G., Olmos, G., & Niñoles, C. L. (2015). The saddle connective tissue graft: a periodontal plastic surgery technique to obtain soft tissue coronal gain on immediate implants-a case report. Int J Esth Dent. 10;444-455.
- Jepsen, K., Stefanini, M., Sanz, M., Zucchelli, G., & Jepsen, S. (2017). Long-term stability of root coverage by coronally advanced flap procedures. J Periodontol. 88; 626-633. https://doi.org/10.1902/jop.2017.160767
- Camargo, P. M., Melnick, P. R., & Kenney, E. B. (2001). The use of free gingival grafts for aesthetic purposes. Periodontol 2000, 27;72- 96. https://doi.org/10.1034/j.1600-0757.2001.027001072.x
- Shkreta, M., Atanasovska-Stojanovska, A., Dollaku, B., & Belazelkoska, Z. (2018). Exploring the Gingival Recession Surgical Treatment Modalities: A Literature Review. Macedoni J Medical Sci. 6; 698-712 https://doi.org/10.3889/oamjms.2018.185
- Sculean, A., Chapple, I. L., & Giannobile, W. V. (2015). Wound models for periodontal and bone regeneration: the role of biologic research. Periodontol 2000. 68;7-20. https://doi.org/10.1111/prd.12091
- Lin, N. H., Gronthos, S., & Mark Bartold, P. (2009). Stem cells and future periodontal regeneration. Periodontol 2000. 51;239-51. https://doi.org/10.1111/j.1600-0757.2009.00303.x
- Jankovic, S., Aleksic, Z., Klokkevold, P., Lekovic, V., Dimitrijevic, B., Barrie Kenney, E., & Camargo, P. (2012). Use of platelet-rich fibrin membrane following treatment of gingival recession: a randomized clinical trial. Int J Period Rest Dent. 32;165-75
- Silva, C. O., Ribeiro, É. D. P., Sallum, A. W., & Tatakis, D. N. (2010). Free gingival grafts: graft shrinkage and donor-site healing in smokers and non-smokers. J Periodontol. 81;692-701. https://doi.org/10.1902/jop.2010.090381
- Susin, C., Fiorini, T., Lee, J., De Stefano, J. A., Dickinson, D. P., & Wikesjö, U. M. (2015). Wound healing following surgical and regenerative periodontal therapy. Periodontol 2000. 68;83-98. https://doi.org/10.1111/prd.12057

