Knowledge, Attitude and Practices Regarding Infection Control Protocol amongst Dental Professionals - A Cross-Sectional Study
OBJECTIVE: The objectives are: (1) to assess and compare the knowledge, attitude and practices regarding infection control protocols and (2) to identify the factor(s) that might influence the implementation of these protocols amongst dental professionals in all three dental campuses of a public sector university, Karachi.
METHODOLOGY: A cross-sectional, observational study was conducted in the three dental campuses of a public sector university, Karachi, for a period of three months from February to April 2019. The study participants consisted of dental and paradental professionals treating patients. A self-administered, structured, validated questionnaire was distributed among 285 participants, out of which 268 participants correctly filled and submitted back the questionnaire. Frequency distribution and Chi square test were performed.
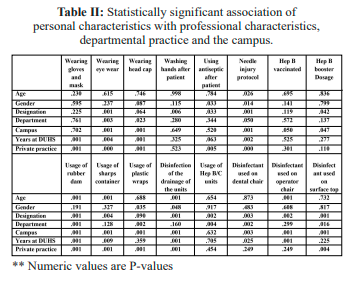
RESULTS: Campus A, covering areas of Mehmoodabad town, Karachi comprising 63 participants; Campus B, covering areas of Saddar town, Karachi comprising 68 participants; and Campus C, covering areas of Gulshan and Johar, Karachi comprising 129 participants, respectively. Statistically significant association was found between eyewear utilization among the designation of the practitioner, dental departments and dental campuses. Correspondingly, significant association was observed between awareness regarding needle stick injury protocol implementation with designation of the practitioner and dental campuses. Likewise, a significant association was found between utilization of rubber dams for maintenance of isolation with the age and designation of the practitioner, dental departments and dental campuses.
CONCLUSION: The study highlighted the shortcomings of infection control protocol implementation in three dental campuses of a premier healthcare university of Pakistan. The results of this study may be utilized provincially and nationally for the construction and effective implementation of infection control policies.
KEYWORDS: AIDS, Disinfection, Hepatitis B, Hepatitis C, Tuberculosis, Needle stick injury.
HOW TO CITE: Azhar R, Ahsan SH, Rasool S, Jamali S, Hussain B. Knowledge, attitude and practices regarding infection control protocol amongst dental professionals - A cross-sectional study. J Pak Dent Assoc 2021;31(1):21-26.
DOI: https://doi.org/10.25301/JPDA.311.21
Received: 30 November 2021, Accepted: 15 September 2021
INTRODUCTION:
Dental professionals are more prone to infectious diseases such as Covid 19, hepatitis B, C, AIDS, tuberculosis, mumps, influenza and rubella1,2 as a result of cross infection, which can be defined as the transmission of infectious agents between patients and staff within a clinical environment3 , during dental examination or procedures.
These diseases can be transmitted directly through contact with blood and aerosol or droplets
(as seen in COVID-19) of infected patients or indirectly by contaminated needle stick injury, improper handling, contaminated surfaces and contact with unsterilized instruments.4,5 Therefore, dental professionals should follow strict infection control protocols not only via instruments sterilization but also disinfect the surrounding objects to ensure safe working environment as these protocols are effective in preventing microbial pollution and cross- contamination and are strongly recommended by worldwide organizations such as the American Dental
Association (ADA), Canadian Dental Association (CDA), the National Health Service (NHS), the Centre for Disease
and Control and Prevention (CDC) and many other health agencies.3,6,7
However, infection control policies in developing countries have not been widely documented 8. Infection
control programs implemented in most dental hospitals of Pakistan are subpar and lack quality assurance measures due to limited awareness of the extent of the problem and absence of properly trained infection control officers.3,8 However, amidst the pandemic (SARS CoV-2), hospitals in Pakistan should improve their infection control programs to curb the spread of COVID-19.
Worldwide studies have been conducted to evaluate infection control protocols followed by dental practitioners
in private and public sectors by accessing their knowledge, attitude and practices. Knowledge, attitude, and practice
(KAP) surveys are representative of a specific population to collect information on what is known, believed and done
in relation to a particular topic and are the most frequently used study tool in research regarding health seeking behavior.9
National survey conducted in Canada in 1999 reported that 46.8% of respondents used extra infection control (IC)
measures for HIV patients and 50.1% for HBV patients 10. However, only 6% of respondents reported excellent compliance with recommended IC procedures which includes but is not limited to attending continuing education about IC in the last two years, treating 20 to 29 patients per day and practicing in a city with a population of > 500,000 10. Till date no such national survey has been conducted in Pakistan.
KAP study conducted in Turkey showed that 96% of dentists preferred to use barrier techniques such as gloves,
masks and protective spectacles, 80% preferred to clean headpieces by wiping them with disinfectants, but only
17.8% preferred sterilized headpieces.3,7 In the same study, 37% participants practiced discarding sharp items utilizing puncture-resistant containers.3
A local KAP study was conducted regarding infection control protocols in Dr. Ishrat-ul-Ebad Khan Institute of Oral Health Sciences (DIKIOHS), Dow University of Health Sciences (DUHS). According to this study, 98% dental
practitioners wore and changed gloves, 74% routinely wore face masks and less than 50% wore protective eyewear
during dental procedures.5 The study also reported that the mean knowledge, attitude and practices regarding infection control protocols were poor among senior dental professionals as compared to house officers and junior dental professionals.5 However, the study did not provide the complete representation of dental professionals in all three campuses of DUHS and therefore comparison of knowledge, attitude and practices among the dental professionals working in different campuses of DUHS was not deciphered.
METHODOLOGY:
We conducted a cross sectional observational study. Ethical approval was taken from the Institutional Review
Board (IRB-1218/DUHS/Approval/2019). The study was conducted in all three dental colleges of DUHS which
comprise of: Campus A, covering areas of Mehmoodabad town, Karachi; Campus B, covering areas of Saddar town,
Karachi and Campus C; covering areas of Gulshan and Johar, Karachi, Pakistan. The study was conducted from February to April 2019. The subjects of the study were dental professionals including dentists, dental hygienists and dental assistants, treating patients at the above-mentioned colleges of DUHS.
The sample size of the study was calculated using an online sample size calculator Open Epi11 (proportion based),
keeping 99% confidence level and 5% confidence limit. According to Pakistan Medical and Dental Council (PM&DC), the total number of dental surgeons and dental specialists registered in Sindh (Pakistan) till January 2018 were 25,299.12 Based on this data, the population size was kept as 25,299. The calculated sample size of the study was
244.11
The exclusion criteria consisted of: 1) Dental faculty members (1st and 2nd year BDS) working in basic health
science departments of DUHS 2) Dental technicians who are not directly involved in treating patients and 3) Bachelor of Dentistry students. (All four years).
A self-made and self-administered questionnaire comprising thirty-one variables regarding infection control
protocols was constructed by the researchers. The questionnaire was based on the criteria which were mentioned
in “Infection prevention checklist for dental settings”, instilled by the Centers of Disease Control and Prevention (CDC) 13. The questionnaire was administered in both English and Urdu languages, according to the preference of the study participant. The questionnaire consisted of three sections namely; “clinical experience”, “personal practice”, and “departmental practice”. The first seven questions were related to socio-demographic details and clinical experience, whereas the remaining questions were utilized to assess the knowledge, attitude and practice of dental professionals regarding infection control protocols, in individual capacity and in their respective department.
Initially, a pilot study was conducted of 10 participants (these participants were excluded from the main study).
Cronbach’s alpha internal reliability test was utilized to determine the internal reliability of the different sections of
the questionnaire. Results showed that by excluding the question “Do you have needle stick injury protocol in your department?” In section III, the Cronbach’s alpha test value of this section improved to 0.782. Therefore, this question was changed to “Do you follow needle stick injury protocol?” and was shifted from section III – Departmental practice to section II – Personal practice, thereby improving the test value of section II to 0.786.
Written consent was taken prior to handing over the questionnaire to the participants. Name and identity of the
participants were not asked to maintain confidentiality. Questionnaires were distributed to n=285 participants in the
three dental colleges of DUHS by the research team. The research team made sure that the subjects were not repeated by maintaining a record of the participants.
For interpretation of the data collected, SPSS version 25 (Chicago, IL, USA) was used. For descriptive analysis, frequency distribution was utilized. For quantitative data, we utilized measures of central tendencies. For qualitative
data, we utilized frequency, percentage, cumulative frequency and cumulative percentage. For inferential statistics we utilized the Chi-square test of independence.
RESULTS:
Two hundred and sixty-eight (n=268) participants returned back the filled questionnaires (response rate = 94%).
The mean age of the participants was 25 years (SD +/-4.00). The gender distribution of participants consisted of 85(31.7%) males and 180(67.2%) females. There were 63 (23.5%) participants from Campus A; 68 (25.4%) participants from Campus B and 129 (48.1%) participants from Campus C that took part in our study. 23(8.6%) participants were from Oral surgery, 47(17.5%) from Operative, 61(22.8%) from Prosthodontics , 31(11.6%) from Orthodontics, 31(11.6%) from Oral diagnosis and 19(7.1%) participants from Periodontology took part in our study respectively. There were 67(25%) paradental staff, 125(46.6%) dental interns, 31 (11.6%) postgraduate trainees and 39(14.6%) faculty members who participated in our study.
Eyewear and Head cap Utilization:
Significant relationship was found between eyewear utilization with designation of the participants (p=0.001), dental
departments (p=0.003), dental campuses (p=0.001) and years of experience of our participants at DUHS (p=0.001).
Dental interns (n=22, 17.6%) and faculty members (n=7, 17.9%) were found to be most compliant with regard to
eyewear utilization whereas postgraduate trainees showed least compliance. Participants of the prosthodontics

 department (n=17, 27%) were most commonly utilizing eyewear while participants of oral surgery (n=9, 39%) and
department (n=17, 27%) were most commonly utilizing eyewear while participants of oral surgery (n=9, 39%) and
oral diagnosis (n=9, 29%) least commonly utilized eyewear as personal protective equipment (PPE).
Results have shown that head cap usage was employed most regularly by the participants of oral diagnosis (n=15,
48%) and operative (n=20, 42.5%) departments and least regularly by the participants of prosthodontics (n=11, 18%)
department. Significant relationship was found between head cap utilization with dental campuses (p=0.001).
Eyewear and head cap utilization was most commonly observed by the participants in campus C (n=34, 26.3%);
(n=30, 23.2%), respectively. In contrast, these practices were least commonly observed by the participants in campus A (n=28, 44.4%); (n=27, 42.8%), respectively, while treating patients.
Awareness of Needle stick injury (NSI) protocol
implementation:
Significant relationship was found between awareness of needle stick injury (NSI) protocol implementation and
designation of the practitioner (p= 0.001), dental departments (p= 0.050) and dental campuses (p= 0.001).
Postgraduate trainees (n=20, 64.5%) were found to be most aware regarding NSI protocol implementation whereas faculty members (n=19, 25.6%) were least commonly aware. In addition, 33.6% (n=42) dental interns reported that they were not aware of this protocol.
Participants in oral surgery (n=15, 65.2%) and operative (n=27, 57.4%) departments were most aware of this protocol, whereas participants in the oral diagnosis (n=11, 35.4%) department were least aware. Campus A comprised 38 (60.4%) participants; campus B comprised 24 (35.2%) participants; and campus C comprised 78 (60.4%) participants who were aware of implementing needle stick injury protocol, after an injury, respectively.
Utilization of sharps disposal container:
Significant relationship was found between utilization of sharps disposal containers and age of the practitioner,
(p=0.001), designation of the practitioner(p=0.004) and dental campuses (p=0.001).
Its utilization was most frequently observed by the participants of campus B (n=66, 97%) and least frequently
observed by the participants of campus A (n=36, 57.1%) for the disposal of sharp objects.
65.6% (n=44) of paradental staff, 93.5% (n=29) of postgraduate trainees; 86.4% (n=108) of dental interns and
74.3% (n=29) of faculty members reported that they always utilized sharps containers. On the contrary, 13.4% (n=9) of the paradental staff reported that they were unaware, while 20.8% (n=14) never utilized sharps disposal containers.
Utilization of plastic wraps:
Significant relationship was found between usage of plastic wraps on the surfaces that came in contact with
dentists/patients with dental departments (p=0.002) and dental campuses (p=0.001).
Participants of oral surgery (n=10, 62.5%) and operative (n=11, 47.8%) departments most frequently changed plastic wraps after every patient while participants of prosthodontics (2.4%) department least frequently changed them.
Utilization of the Rubber dam for isolation:
Significant relationship was found between rubber dam usage and age of the practitioner (p=0.001), designation of
the practitioner (p=0.001), dental departments (p=0.001), dental campuses (p= 0.001) and years of experience at DUHS (p= 0.001).
Its utilization was most frequently observed by the participants of campus C (n=91, 70.5%) and least frequently
by the participants of campus B (n=11, 16.1%) for maintenance of isolation.
Dental interns (n=64, 50%) most frequently utilized rubber dams whereas faculty members (n=5, 3.9%) least
frequently utilized them.
Insignificant relationship was found between sterilization of instruments with age, gender and designation of the
practitioner, dental departments and dental campuses. Furthermore, an insignificant relationship was found between washing of hands after every patient and age, gender and designation of the practitioner, dental departments and campuses. However, it was noticed that washing hands regularly was most commonly practiced by the dental interns (n=87, 69.6%) and least commonly practiced by the postgraduate trainees (n=18, 58%).
Similarly, no significant relationship was found between Hepatitis B vaccination and booster vaccination with age,
gender and designation of the practitioner, dental departments and campuses. However, 22.5% (n=7) of postgraduate trainees; 28.2% (n=11) of faculty members; 32.8% (n=41) of dental interns and 50.7% (n=34) of paradental staff reported that they didn’t have booster vaccination.
DISCUSSION:
Awareness of infection control protocols is of paramount importance as it plays a pivotal role in the prevention of
spread of infectious and transmissible diseases. Dental professionals including dental auxiliaries should therefore be aware of these protocols. Dow University of Health Sciences (DUHS) is now focusing on implementing the infection control policy according to the national guideline for infection prevention and control, ministry of health, Pakistan.14 This study attempted to assess the knowledge, attitude and practices of dental professionals regarding the infection control in all the three campuses of DUHS.
Personal protective equipment (PPE), which includes protective clothing, gloves, masks, eyewear and head covering provides protection and control against infections.7,15 Our study reported highest compliance in wearing gloves and masks (93.7%) and lowest compliance with wearing protective eyewear (19%) and head cap (14.6%) and
in accordance with the study of Halboub et al15 and Malhotra et al18 who also reported similar results in studies
conducted in Yemen and India respectively.
Dagher et al20 reported protective eyewear and head coverings being least implemented protocol among dentists
in Lebanon. These unsatisfactory results indicate decreased awareness regarding infection transmission via aerosols and blood splashes among dental professionals.15 The present study observed dental interns to be most compliant, which reflects that they were constantly encouraged to follow these universal precautions during their internship training. The department of Oral diagnosis was shown to be least compliant, which reflects their poor attitude in following these universal precautions, despite being exposed to most patients.
Hand washing is the single most effective barrier towards infection control.21,22 Our study reported substantial conformity of hand washing among dental professionals (76.5%) after every patient. Malhotra et al18 stated perfect
compliance (100%) among dental students in Patiala, India. Decreased compliance may result from the fact that dental professionals consider wearing gloves as an effective measure
for infection control. However, gloves have micropores,
which are an important mode of transmission for infectious
agents.
The findings of the present study indicated most (88.4%) of the dental practitioners were Hepatitis B (HBV) vaccinated. These results were significantly higher than reported by Halboub et al15 in the Yemeni population (70.7%) but lower than reported by Alharbi et al16 in the Saudi population (93.1%) and other studies conducted in Brazil (91%) and Canada (100%).15 The current study also revealed a significant decrease (54.1%) when recommended booster dose was investigated, compared to Rahman et al (64.7%) in UAE and De Souza et al (83.3%) in Brazil.15,23,24 The present authors observed that paradental staff had the lowest rate (38.8%) of HBV vaccination, which is in agreement with previous study conducted by Sohail et al17 among dental auxiliaries in Islamabad (52%). These higher frequencies indicate that countries such as Canada, Brazil and Saudi Arabia have mandatory policies for Hepatitis B vaccination prior to clinical practice for dental students, faculty members
and staff.12 Lack of infection control policies and awareness regarding booster dose of Hepatitis B vaccine are important factors which contribute towards the low rates of vaccination in the present study.
Needle stick injury (NSI) is the most common route of transmission for blood-borne diseases among dental healthcare workers.25,26 Our study reported only 54.1% of dental practitioners being aware of having NSI protocol after an injury. Similar results were reported by Malik et al which reported that most of the dental practitioners (74%) were aware of the universal NSI precautions, however, the overall practice of infection control procedures was found to be unsatisfactory.27 This reflects the lack of universally applied NSI protocol provided by government-based health policy organizations in Pakistan. In addition to that, most of the institutes also do not follow any NSI protocol which is alarming considering the fact that NSI are more prevalent in the dental environment than any other health care setting.15,24 The present authors observed post graduate trainees were most aware of this protocol. This reflects that the post graduate training in DUHS provides awareness regarding the prevention and management of NSI.
Our study also compared the knowledge, attitude and practices regarding infection control protocol of the three
dental campuses of DUHS. Our study revealed that campuses B and C were found to be more compliant as compared to campus A, which reflects stronger policies regarding infection control protocol implementation.
Limitation of the study is that survey-based studies are subject to bias, based on the fact that a filled questionnaire
can consist of either a pseudo positive or a pseudo negative response. Therefore, the responses might not accurately
reflect the true knowledge, attitude and practices of the subjects. In addition to that, a cross sectional study design
cannot measure the change, based on gradual increase in awareness of the society.
DISCLAIMER:
This manuscript is not presented or published in any
conference or journal. It is not part of a PhD thesis.
CONFLICT OF INTEREST:
None to declare
FUNDING DISCLOSURE:
None to declare
REFERENCES:
1. Araujo MW, Andreana S. Risk and prevention of transmission of infectious diseases in dentistry. Quintessence Int. 2002;33:376-82.
2. Askarian M, Assadian O. Infection control practices among dental professionals in Shiraz Dentistry School, Iran. Arch Iran Med. 2009;12:48-51.
3. Y¼zbasioglu E, Saraç D, Canbaz S, Sara YS, Cengiz S. A survey of cross-infection control procedures: knowledge and attitudes of Turkish dentists. J Appl Oral Sci. 2009;17:565-9.
https://doi.org/10.1590/S1678-77572009000600005
4. Abichandani S, Nadiger R. Cross contamination in dentistry: A comprehensive overview. J. educ. ethics dent. 2012;2:3.
https://doi.org/10.4103/0974-7761.115139
5. Mohiuddin S, Dawani N. Knowledge, attitude and practice of infection control measures among dental practitioners in public setup of Karachi, Pakistan: cross-sectional survey. J Dow Univ Health Sci. 2015;9.
6. Centers for Disease Control (CDC). Update: transmission of HIV infection during invasive dental procedures–Florida. MMWR. Morb Mortal Wkly Rep. 199;40:377-81.
7. Kohn WG, Harte JA, Malvitz DM, Collins AS, Cleveland JL, Eklund KJ. Cover story guidelines for infection control in dental health care settings-2003. J. Am. Dent. Assoc. 2004;135:33-47.
https://doi.org/10.14219/jada.archive.2004.0019
8. Morris E, Hassan FS, Al Nafisi A, Sugathan TN. Infection control knowledge and practices in Kuwait: a survey on oral health care workers. Saudi Dent J. 1996;8:699-703.
9. ul Haq N, Hassali MA, Shafie AA, Saleem F, Farooqui M, Aljadhey H. A cross sectional assessment of knowledge, attitude and practice towards Hepatitis B among healthy population of Quetta, Pakistan. BMC Public Health. 2012;12:1-8.
https://doi.org/10.1186/1471-2458-12-692
10. McCarthy GM, Koval JJ, MacDonald JK. Compliance with recommended infection control procedures among Canadian dentists: results of a national survey. Am. J. Infect. Control. 1999;27:377-84.
https://doi.org/10.1016/S0196-6553(99)70001-5
11. Anon, (2020). [online] Available at: https://www.openepi.com/ SampleSize/SSPropor.htm [Accessed 18 Feb. 2020].
12. Pmdc.org.pk. (2020). Welcome to PMC. [online] Available at: http://www.pmdc.org.pk/Statistics/tabid/103/Default.aspx [Accessed10 Dec, 2018].
13. Cdc.gov. 2021. Appendix A: Infection Prevention Checklist for Dental Settings: Basic Expectations for Safe Care. [online] Available
at: <https://www.cdc.gov/oralhealth/infectioncontrol/summaryinfection-prevention-practices/appendix-a.html> [Accessed 26 August 2021].
14. National Institute of Health Islamabad. 2021. National Guidelines: Infection Prevention & Control – National Institute of Health Islamabad.
[online] Available at: <https://www.nih.org.pk/national-guidelinesinfection-prevention-control/> [Accessed 26 August 2021].
15. Halboub ES, Al-Maweri SA, Al-Jamaei AA, Tarakji B, Al-Soneidar WA. Knowledge, attitudes, and practice of infection control among dental students at Sana’a University, Yemen. Int. J. Oral Health Dent. 2015;7:15.
https://doi.org/10.4103/2231-0762.156152
16. Alharbi G, Shono N, Alballaa L, Aloufi A. Knowledge, attitude and compliance of infection control guidelines among dental faculty members and students in KSU. BMC oral health. 2019;19:7.
https://doi.org/10.1186/s12903-018-0706-0
17. Sohail S, Jamal M, Bari WG, Saleem MM. KNowledge, attitude and working habits concerning infection control measures among dental staff of islamabad dental hospital. Pak Oral Dental J. 2019;39:164-6.
18. Malhotra V, Kaura S, Sharma H. Knowledge, attitude and practices about hepatitis B and Infection Control Measures among dental students in Patiala. J. Dent Allied Sci. 2017;6:65.
https://doi.org/10.4103/2277-4696.219977
19. Alhowaish MA, Alhowaish JA, Alanazi YH, Alshammari MM, Alshammari MS, Alshamari NG, Alshammari AS, Almutairi MK, Algarni SA. Knowledge, attitudes and practices toward prevention of hepatitis B virus infection among medical students at Northern Border University, Arar, Kingdom of Saudi Arabia. Electronic physician. 2017;9:5388.
https://doi.org/10.19082/5388
20. Dagher J, Sfeir C, Abdallah A, Majzoub Z. Infection control measures in private dental clinics in Lebanon. Int. J. Dent. 2017.
https://doi.org/10.1155/2017/5057248
21. Omogbai JJ, Azodo CC, Ehizele AO, Umoh A. Hand hygiene amongst dental professionals in a tertiary dental clinic. African J. Clin. Exp. Microbiol. 2011;12.
https://doi.org/10.4314/ajcem.v12i1.61040
22. Al-Naggar RA, Al-Jashamy K. Perceptions and barriers of hands hygiene practice among medical science students in a medical school in Malaysia. IIUM Int. Med. J. Malays. 2013;12.
https://doi.org/10.31436/imjm.v12i2.503
23. Rahman B, Abraham SB, Alsalami AM, Alkhaja FE, Najem SI. Attitudes and practices of infection control among senior dental students at college of dentistry, university of Sharjah in the United Arab Emirates. Eur J Dent. 2013;7(S 01):S015-9.
https://doi.org/10.4103/1305-7456.119058
24. de Souza RA, Namen FM, Galan J Jr, Vieira C, SedanoHO. Infection control measures among senior dental students in Rio de Janeiro State, Brazil. J Public Health Dent 2006;66:282-4.
https://doi.org/10.1111/j.1752-7325.2006.tb04084.x
25. Lee JJ, Kok SH, Cheng SJ, Lin LD, Lin CP. Needlestick and sharps injuries among dental healthcare workers at a university hospital. J Formos Med Assoc. 2014;113:227-33.
https://doi.org/10.1016/j.jfma.2012.05.009
26. Zafar A, Aslam N, Nasir N, Meraj R, Mehraj V. Knowledge, attitudes and practices of health care workers regarding needle stick injuries at a tertiary care hospital in Pakistan. J Pak Med Assoc. 2008;58:57-60.
27. Malik A, Shaukat MS, Qureshi A. Needle-stick injury: A rising bio-hazard. J Ayub Med Coll Abbottabad. 2012;24:144-6.

