One Point Fixation Versus Two Point Fixation in Zygomaticomaxillary Complex Fractures
OBJECTIVE: To compare the mean satisfaction of patients undergoing one point fixation versus two point fixation for zygomaticomaxillary complex fractures.
METHODOLOGY: This randomized controlled trial was performed at Oral and Maxillofacial surgey department Punjab Dental Hospital. The duration of this study was 6 months (28-8-18 to 28-2-19). After meeting the inclusion criteria 74 patients were enrolled. Informed consent and demographic information was taken. Patients were randomly divided into two groups. One group is treated with one point fixation method and other with two point fixation. Patient were evaluated in terms of satisfaction of score on 3rd day, 14th day and 28th day and were recorded as per operational definitions. All the collected data was entered and analyzed on SPSS version 20.
RESULTS: In this study the mean age of patients in one point group was 42.46±15.325 years while in two points group was 49.32±13.145 years, male to female ratio of the patients was 1.2:1. The mean PSS in one point group was 5.98±0.89 while in two points group was 3.775±0.609 (p-value=<0.001).
CONCLUSION: One point fixation is smarter method and provide significantly better satisfaction than to two point fixation method for ZMC fractures
KEYWORDS: Zygomaticomaxillary Complex Fractures, One Point, Two Point, Satisfaction
HOW TO CITE: Akram MH, Ch MM, Mirza AI, Akhtar MU, Saeed A. One point fixation versus two point fixation in zygomaticomaxillary complex fractures. J Pak Dent Assoc 2021;30(2):74-80.
DOI: https://doi.org/10.25301/JPDA.302.74
Received: 16 September 2020, Accepted: 25 December 2020
INTRODUCTION:
Chronic periodontitis (CP), an inflammatory condition of supporting structures of teeth, that affects more than 75% of the adult population of hronic periodontitis (CP), an inflammatory condition of supporting structures of teeth, that affects more than 75% of the adult population of obstructive pulmonary disease and kidney disease.6 The goal of the periodontal treatment is to limit microbial invasion into periodontal tissues by controlling plaque and calculus deposits at early stages through scaling and/or root planning, followed by at home use of teeth-cleaning aids such as dentifrices and mouthwashes.
obstructive pulmonary disease and kidney disease.6 The goal of the periodontal treatment is to limit microbial invasion into periodontal tissues by controlling plaque and calculus deposits at early stages through scaling and/or root planning, followed by at home use of teeth-cleaning aids such as dentifrices and mouthwashes.
METHODOLOGY:
We have recently published the detailed methodology of this parallel-arm randomized controlled trial that was conducted at Department of Periodontology, FMH College of Medicine & Dentistry, Lahore Pakistan from January 2018 to June 2019, after ethical approval from the institutional ethical committee vide letter number FMH[1]07-2017-IRB-268-F.13,14 The trial was registered with clinicaltrials.gov (NCT03270280) and followed the CONSORT guidelines.13,14 The duration of clinical use of mouthwash in this trial was two weeks and details regarding inclusion and exclusion criteria, consent approval, blinding procedure, flow charts etc have been described in our recent publications.13,14 The sample size was calculated by using the following comparison of mean formula keeping the power of study at 90% and and 5% margin of error based on published values of one of the variables (MMP-8) of the study.
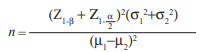
We have recently published the detailed methodology of this parallel-arm randomized controlled trial that was conducted at Department of Periodontology, FMH College of Medicine & Dentistry, Lahore Pakistan from January 2018 to June 2019, after ethical approval from the institutional ethical committee vide letter number FMH[1]07-2017-IRB-268-F.13,14 The trial was registered with clinicaltrials.gov (NCT03270280) and followed the CONSORT guidelines.13,14 The duration of clinical use of mouthwash in this trial was two weeks and details regarding inclusion and exclusion criteria, consent approval, blinding procedure, flow charts etc have been described in our recent publications.13,14 The sample size was calculated by using the following comparison of mean formula keeping the power of study at 90% and and 5% margin of error based on published values of one of the variables (MMP-8) of the study.
The recommended dose of NS oil-based mouthwash for this study was calculated as 500 mg (five ml or fifty-five drops) of NS oil, as per previously published. 13,14,16 Same amount was recommended for normal saline solution that was designated as a placebo in this study. A total of eighty ml of NS oil and the normal saline mouthwashes were dispensed in amber bottles which were sequentially numbered and triple blinding was ensured to avoid any bias in the study.
The recommended dose of NS oil-based mouthwash for this study was calculated as 500 mg (five ml or fifty-five drops) of NS oil, as per previously published. 13,14,16 Same amount was recommended for normal saline solution that was designated as a placebo in this study. A total of eighty ml of NS oil and the normal saline mouthwashes were dispensed in amber bottles which were sequentially numbered and triple blinding was ensured to avoid any bias in the study.
STATISTICAL ANALYSIS:
All the collected data was coded and analyzed using IBM Statistical Package for the Social Sciences (SPSS, Version 25.0). The variables of age, CAL, PPD, PI, and BoP were presented as means and standard deviations (SDs). Wilcoxon signed-rank test was used to compare the pre-treatment and post-treatment changes in mean values of these clinical periodontal parameters within both the groups while Mann Whitney-U test was computed to observe the differences in periodontal parameters between the two study groups. For all analysis, p value of < 0.05 was considered statistically significant.
RESULTS:
As reported previously, a total of forty participants (twenty in each group) completed the study till the end hence a loss to follow-up of twenty percent was observed. The mean of age of the study participants in treatment group and control group was 36.39±8.14 years and 38.27±7.44 years respectively.
The pre-treatment and post-treatment changes in the mean values of clinical CP parameters within both the groups were analyzed. It was noted that a statistically significant difference was found in the pre-treatment and post-treatment values of all CP parameters in both the groups (Table 1). This indicated that the clinical CP parameters improved in both the treatment and the control groups irrespective of the mouthwash used.
Table 1: Comparison of Clinical Parameters of Chronic Periodontitis before and After Treatment within Each Study Group
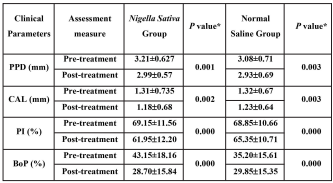
Upon comparison of clinical parameters within the group, a statistically significant value is observed for all clinical parameters in both the groups. PPD: Periodontal Pocket Depth, CAL: Clinical Attachment Loss, PI: Plaque Index, BoP: Bleeding on Probing. * Level of Significance.
Table 2: Comparison of Pre-treatment and Post-treatment Values of Clinical Parameters of Chronic Periodontitis between Treatment and Control groups
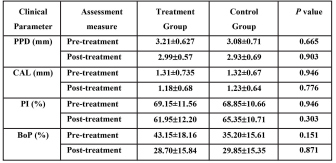
PPD: Periodontal Pocket Depth, CAL: Clinical Attachment Loss, PI: Plaque Index, BoP: Bleeding on Probing. All the clinical parameters of pre-treatment groups except BoP are almost similar in both the study groups. *Level of significance
Using Mann Whitney-U test (Table 2) the mean values of clinical parameters of CP before treatment were similar so the two groups had the same severity of CP at the baseline. The post-treatment PPD, CAL, PI and BoP values of control & treatment groups have been shown in table 2 and the findings highlighted that the difference in improvement of periodontal health between the treatment and control group was not statistically significant, indicating that periodontal health improved in both trial arms with no difference between groups after two weeks of use of NS oil-based or normal saline-based mouthwashes.
DISCUSSION:
The World Health Organization (WHO) has advocated the use of medicinal plants in treatment of any disease condition owing to their promising results and fewer side effects. The organization also encourages developing countries to use medicinal plants as a resource in their health care systems.8 Keeping in view the anti-inflammatory and anti-microbial potential of NS in mind, we investigated the efficacy of NS oil-based mouthwash as an adjunct therapy measure for unhealthy periodontium for two weeks after initial scaling and root planning. We used normal saline as placebo adjuvant solution in our control group. Interestingly, following scaling and root planning, we found that use of both normal saline mouthwash and NS oil-based mouthwash had statistically significant results regarding improvement in the clinical parameters of CP after two weeks of usage. These results can have two potential implications, one that that both NS oil and normal saline solution have a beneficial effect on improvement of clinical periodontal parameters and two that clinical periodontal parameters improve due to the non-surgical periodontal therapy and any mouthwash used would have a limited effect.
As for the effectiveness of NS oil-based mouthwash in the present study, other studies support the claim. A study compared the efficacy of mucoadhesive TQ gel mucoadhesive NS extract after scaling and root planning in chronic periodontitis patients. It was found that the use of adjunct treatment to mechanical debridement was more effective in treatment of chronic periodontitis as compared to mechanical treatment by scaling and root planning alone.17 It has also been shown that application of a biodegradable periodontal chip containing TQ for sixty days following conventional scaling and root planning significantly reduced clinical periodontal parameters of CP in patients as compared to the chlorhexidine group. This study advocated the use of TQ-based chips in chronic periodontitis patients as an adjunctive therapy during the scaling and root planning, or for follow-up visits.18 Another study also reported an improvement in clinical parameters of CP after scaling and root planning followed by use of TQ gel in patients with CP as compared to patients undergoing scaling and root planning alone. The results of this study indicated the importance of NS in periodontal treatment even after scaling and root planing.19 Similarly, another study found the use of TQ gel in chronic periodontitis patients significantly led to improvement of parameters of CP as compared to those patients that had only scaling and root planning done. This indicated that use of NS oil also leads to improvement in clinical parameters of CP.20
As regards to normal saline-based mouthwashes, there is mixed data available. Normal saline solution is commonly used as a gargle-based home remedy for conditions such as cough, sore throat and as a mouthwash for oral ulcers.21 An in vitro study advocated the use of short-term rinsing with saline mouthwash solution for improvement of oral health. This study showed the saline solution promoted human gingival fibroblasts migration and increased the expression of extracellular matrix including collagen-I and cytoskeletal proteins such as F-actin.22 Another study compared the effectiveness of use of normal saline and chlorhexidine for five days in reducing dental plaque in patients with chronic periodontitis. The use of normal saline solution proved to be as effective as chlorhexidine and thus the authors suggested that saline mouthwash rinse can be utilized as an adjunct measure for plaque control and promotion of oral health.21 Our study has also suggested the normal saline solution can be an effective measure for improvement in all clinical parameters of CP after initial scaling and root planning has been performed.
The second implication is that both the mouthwashes had a negligible effect on the improvement of clinical periodontal parameters which would have been improved even after simple use of sub-gingival ultrasonic instrumentation (SUI) for scaling and root planning as SUI is in itself reported as an effective measure in removing the periodontal bacteria thus improving healing in the deeper periodontal tissues.23,24 Following SUI, different studies have employed the use of mouthwashes including normal saline, povidone-iodine, chlorhexidine and some essential oils ranging in follow-up from two weeks to six months but all the studies did not find any difference in the type of mouthwash used for healing and concluded that the use of SUI through sub-gingival plaque removal and bacterial cell disruption achieved by the vibrating chipping action of the scaler tip, cavitational activity, and acoustic micro-streaming alone is effective for controlling and treating periodontal disease.23-25 In our study, we also performed scaling and root planning and then patients were advised to apply a minimal amount of NS oil or normal saline solution to their gingiva for two weeks. It is possible that we found an improvement in clinical parameters just due to performing of SUI. This also suggested the possibility that the improvement of clinical parameters of CP in our study could be due to the role of scaling and root planning alone without any adjunct therapy mouthwashes, however, the limitations of the current findings was the use of NS oil mouthwash for only two weeks duration and therefore results cannot be generalized for longer duration studies. Future studies on NS oil may focus on increased sample sizes and longer duration use with follow-up at different time points.
CONCLUSION:
It is concluded that the clinical periodontal parameters of PI, CAL, PPD and BoP in the present study improved after two weeks following non-surgical periodontal therapy in both CP groups using NS oil-based mouthwash and normal saline-based mouthwashes. Thus either both mouthwashes had a beneficial effect on clinical parameters or non-surgical periodontal therapy itself was enough for improvement of periodontal health irrespective of the mouthwash used.
ACKNOWLEDGMENTS:
We are thankful to all the voluntary study participants that contributed valuable data for this study. We would also like thank to the clinical staff at the periodontology department, Fatima Memorial Hospital, Shadman, Lahore and the staff at Oral Biology department, University of Health Sciences Lahore, regarding their support for the study
FUNDING DISCLOSURE:
The M. Phil studies and financial support of the project for GH was fully funded by the University of Health Sciences, Lahore.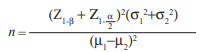
AUTHORS’ CONTRIBUTION:
GH did experiments and manuscript writing.
SG conceived, designed, did manuscript writing, provided critical revisions through intellectual output and did final approval of the manuscript.
SA provided critical revisions through intellectual output and did manuscript writing
ZAK provided clinical assistance and gave intellectual output during the sampling procedure
CONFLICT OF INTEREST:
The authors have no conflict of interest
REFERENCES:
- Amin M, Amanullah BM, Tarar AM. Dental caries, periodontal disease and their associated factors among patients visiting dental Teaching Hospital in Multan, Pakistan. J Pak Dent Assoc. 2016;25: 98-102.
- Amin M, Amanullah BM, Tarar AM. Dental caries, periodontal disease and their associated factors among patients visiting dental Teaching Hospital in Multan, Pakistan. J Pak Dent Assoc. 2016;25: 98-102.
- Khan S, Khalid T, Awan KH. Chronic periodontitis and smoking Prevalence and dose-response relationship. Saudi Med J. 2016;37:889- 94. https://doi.org/10.15537/smj.2016.8.14223
- Cardoso EM, Reis C, Manzanares-Céspedes MC. Chronic periodontitis, inflammatory cytokines, and interrelationship with other chronic diseases. Postgrad Med. 2018;130:98-104. https://doi.org/10.1080/00325481.2018.1396876
- Kinane DF, Stathopoulou PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Primers. 2017;3:1-14. https://doi.org/10.1038/nrdp.2017.38
- Hickey NA, Shalamanova L, Whitehead KA, Dempsey-Hibbert N, van der Gast C, Taylor RL. Exploring the putative interactions between chronic kidney disease and chronic periodontitis. Crit Rev Microbiol. 2020;46:61-77. https://doi.org/10.1080/1040841X.2020.1724872
- Machado V, Lobo S, Proença L, Mendes JJ, Botelho J. Vitamin D and Periodontitis: A Systematic Review and Meta-Analysis. Nutrients. 2020;12:2177. (Page 1-18) https://doi.org/10.3390/nu12082177
- Hassan G, Ghafoor S. Herbal Medicines: An Adjunct to Current Treatment Modalities for Periodontal Diseases. Biomedica. 2020;36: 15-22.
- Ozdemir H, Kara M, Erciyas K, Ozer H, Ay S. Preventive effects of thymoquinone in a rat periodontitis model: a morphometric and histopathological study. J Periodont Res 2012;47:74-80. https://doi.org/10.1111/j.1600-0765.2011.01406.x
- Al-Wafi HA. Benefits of Thymoquinone, a Nigella Sativa Extract in Preventing Dental Caries Initiation and Improving Gingival Health: Tufts University School of Dental Medicine; 2014. (Page 1-73)
- . AlHarthi S, AlTamimi M, AlDreib H, AlAgeel L, Binshabaib M, Rahman I. Nigella sativa Mouthwash’s antimicrobial properties make it a viable candidate for development of a natural alternative to chlorhexidine. Int J Herb Med 2020.
- Senthilnathan K, Ilango P, Abirami T, Vummidi VA, Mahalingam AP, Reddy VK. Evaluation of antibacterial activity of Nigella sativa seed extract against Porphyromonas gingivalis and Prevotella intermedia. J Interdiscip Dent. 2020;10:51. https://doi.org/10.4103/jid.jid_62_19
- Hassan G, Ghafoor S, Chaudhry S, Khan ZA. Effect of Nigella Sativa (Kalonji) Oil Based Mouth Wash on Salivary Matrix Metalloproteinase-8 Levels in Patients with Chronic Periodontitis. A Randomized Controlled Trial. Biomedica. 2020;36:285-90
- Hassan G, Ghafoor S, Chaudhry S, Khan ZA. Salivary Interleukin[1]1 Levels in Chronic Periodontitis Patients after use of Nigella Sativa (Kalonji) Oil. J Pak Dent Assoc. 2020;29:205-10. https://doi.org/10.25301/JPDA.294.205
- Gupta N, Gupta N, Gupta A, Khan S, Bansal N. Role of salivary matrix metalloproteinase-8 (MMP-8) in chronic periodontitis diagnosis. Frontiers of medicine. 2015;9:72-6. https://doi.org/10.1007/s11684-014-0347-x
- Tasawar Z, Siraj Z, Ahmad N, Lashari MH. The effects of Nigella sativa (Kalonji) on lipid profile in patients with stable coronary artery disease in Multan, Pakistan. Pakistan J Nutr. 2011. https://doi.org/10.3923/pjn.2011.162.167
- Fatehi B, Ziaie N. Effect of Mucoadhesive Nigella sativa on Treatment of Chronic Periodontitis. J Periodontol Implant Dent. 2018;10.
- Al-Bayaty FH, Kamaruddin AA, Ismail M, Abdulla MA. Formulation and evaluation of a new biodegradable periodontal chip containing thymoquinone in a chitosan base for the management of chronic periodontitis. J Nanomater. 2013; Article ID 397308. https://doi.org/10.1186/ISRCTN29742423
- Kapil H, Suresh D, Bathla SC, Arora KS. Assessment of clinical efficacy of locally delivered 0.2% Thymoquinone gel in the treatment of periodontitis. Saudi Dent J. 2018;30:348-54. https://doi.org/10.1016/j.sdentj.2018.06.001
- Alaaeldin E, Gomaa MD, Eltewacy NK, Ali A, Khalil AA. Formulation and Characterization of Thymoquinone Bioadhesive Gel for Treatment of Chronic Gum Inflammation. Int J Sci Basic Appl Res. 2017;31:321-30
- Aravinth V, Narayanan MA, Kumar SR, Selvamary AL, Sujatha A. Comparative evaluation of salt water rinse with chlorhexidine against oral microbes: A school-based randomized controlled trial. J Indian Soc Pedod Prev Dent. 2017;35:319-26. https://doi.org/10.4103/JISPPD.JISPPD_299_16
- Huynh NC-N, Everts V, Leethanakul C, Pavasant P, Ampornaramveth RS. Rinsing with saline promotes human gingival fibroblast wound healing in vitro. PloS one. 2016;11:e0159843. https://doi.org/10.1371/journal.pone.0159843
- Morozumi T, Kubota T, Abe D, Shimizu T, Nohno K, Yoshie H. 85 Efficacy of normal saline and Nigella Sativa on clinical periodontal parameters JPDA Vol. 30 No. 02 Apr-Jun 2021 Hassan G/ Ghafoor S/ Atif S/ Chaudhry S/ Khan ZA Microbiological effect of essential oils in combination with subgingival ultrasonic instrumentation and mouth rinsing in chronic periodontitis patients. Int J Dent. 2013;2013. https://doi.org/10.1155/2013/146479
- Lavanchy DL, Bickel M, Baehni P. The effect of plaque control after scaling and root planing on the subgingival microflora in human periodontitis. J Clin Periodontol. 1987;14:295-9. https://doi.org/10.1111/j.1600-051X.1987.tb01536.x
- Leonhardt , Bergstrm C, Krok L, Cardaropoli G. Microbiological effect of the use of an ultrasonic device and iodine irrigation in patients with severe chronic periodontal disease: a randomized controlled clinical study. Acta Odontologica Scandinavica. 2007;65:52-9. https://doi.org/10.1080/00016350600973078

