The Pattern Of Diagnosis Of Oral Soft Tissue Biopsies In Saudi Arabian Children And Adolescents
OBJECTIVE: Oral diseases have a variable epidemiology from region to region. There is paucity of reports on the range of diagnoses regarding soft tissue biopsies in pediatric patients in Saudi Arabia.
AIM: The study aimed to determine the frequency of histologically diagnosed lesions in softtissue biopsy specimens of patients between the ages of 0-18 years in a Saudi Arabian teaching hospital over a 30 year period.
METHODOLOGY: The histopathology diagnoses records with complete demographic data of pediatric patients whose soft tissue biopsies were diagnosed in the Histopathology laboratory of College of Dentistry, King Saud University, Saudi Arabia between 1984 and 2013 were retrieved and reviewed, alongside their histopathology slides. The lesions were then classified into 8 broad categories.
RESULTS: A total of 280 pediatric soft tissue biopsies diagnosed during this period had complete records. The male to female ratio was 0.74 and mean age was 12 years. Reactive lesions were most commonly seen (51.1%) followed by salivary gland lesions (26.4%). The most common specific lesions were pyogenic granuloma, mucous extravasation cysts and fibroma. The sites most commonly affected were gingiva, lips, buccal mucosa and tongue.
CONCLUSION: Oral soft tissue lesions in Saudi children were predominantly reactive and benignin nature and the frequencies of observed lesions are not significantly different from those from studies from other parts of the world despite relative cultural and environmental influences that would be expected to play a role in the prevalence of specific lesions.
HOW TO CITE: Qannam A. The Pattern of Diagnosis of Oral Soft Tissue Biopsies in Saudi Arabian Children and Adolescents.
J Pak Dent Assoc 2015; 24(2):93-99.
INTRODUCTION
Although children suffer from manyoral diseases found in adults there are undoubtedly some difference in prevalence of various lesions in comparison to the latter1. In addition, there are lesions relatively unique to the pediatric population2,3. There have been various studies on the frequency of oral lesions in children from various continents of the world.These studies have highlighted differences in racial and regional differences in the prevalence of oral lesions4-14. A common denominator with all the studies is the lack of unanimity in defining what constitutes the pediatric age group, in the classification of various disease entities and in the time period over which the data was collected8. This lack of unanimity in study design makes it difficult to make relatively valid comparison between studies.In dentistry, the pediatric age is generally considered as between 0-18 years, encompassing such periods as the infancy, childhood and adolescence.
Most of the previous studies have reported biopsies involving hard and soft tissues although a few have concentrated on specific group of lesions such as salivary gland lesions15, odontogenic16,17 and non-odontogenic tumors18. There has been no study dedicated to examining only the range of diagnosis of soft tissue lesions in children. Most previous studies have reported them in the context of all lesions including hard tissue and dental lesions.With this method there is a strong likelihood that soft tissue lesions are often overlooked19.
Studies on soft tissue lesions19,20 are often based mainly on clinical examinations as the only tool for diagnosis. Although a substantial proportion of soft tissue lesions do not require tissue biopsies, many of them are only conclusively diagnosed histologically. Therefore a study of the range of diagnoses of soft tissue lesions submitted to an oral pathology service will complement those based on clinical diagnoses in giving a true picture of soft tissue lesions in children. This will probably have greater influence in designing a more coherent public health policy for tackling oral disease in pediatric patients.
With the knowledge that similar studies have not been undertaken previously in Saudi Arabia,this study aimed to determine the frequency of soft tissue lesions histologicallydiagnosed and relate this to the age (age group), gender and site of the biopsy in patients between 0 and 18 years old in the College of Dentistry, King Saud University over a 30 year period (1984-2013). An additional aim is to make a comparison with the soft tissue biopsies in previous reports of pediatric oral lesions in the English literature.
METHODOLOGY
Study Setting
The setting of the study is the biopsy service at the College of Dentistry, King Saud University, Riyadh, Saudi Arabia. Many of the cases come from university staff and relations, the general public and a few of them seen as cases for consultation from other centers that also run their own biopsy services.Ethical permission was sought and obtained from the local Institutional Review Board (College of Dentistry Research Center, FR 0181).
General Evaluation
The biopsy records of patients between 0 and 18 years of age were retrieved from the archives
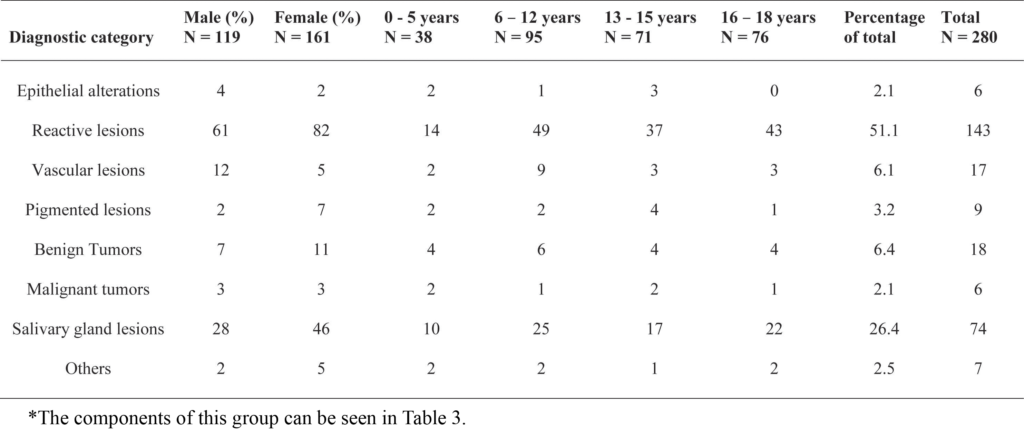 Table 1: General categorization of lesions relative to gender and age grouping
Table 1: General categorization of lesions relative to gender and age grouping
of the above named service spanning the period 1984 to 2013. All cases that were reported as soft tissue lesions with complete record of the patient’s gender, anatomic site of lesion and histopathologic diagnosis clearly stated were included in this study.As the author alongside a colleague arepracticing oral pathologists, all slides (including those with special stains and immunohistochemical staining) were then recalled to re-check the histopathologic diagnoses. New diagnoses based on current knowledge were reassigned to many lesions including to those cases with previously inconclusive diagnoses, where possible.Data was presented as frequencies and percentages. Associations between variables were tested by Pearson chi-square test or Fisher’s exact test where necessary. A p value of less than 0.05 was considered statistically significant. Analyses was done using IBM SPSS software version 20.
RESULTS
Two hundred and eighty patients comprising 119 (42.5%) males and 161(57.5%) females met the inclusion criteria for this study. The mean age of the study subjects was 12 years (range: 2 weeks to 18 years). Majority of the specimens were obtained from the age group 6-12 years (Table 1). Most lesions were located in the gingiva, the lips, buccal mucosa and the tongue (Table 2). Among the categories of lesions, reactive lesions accounted for slightly more than half (51%) of the biopsies reported in this study group followed by salivary gland-related
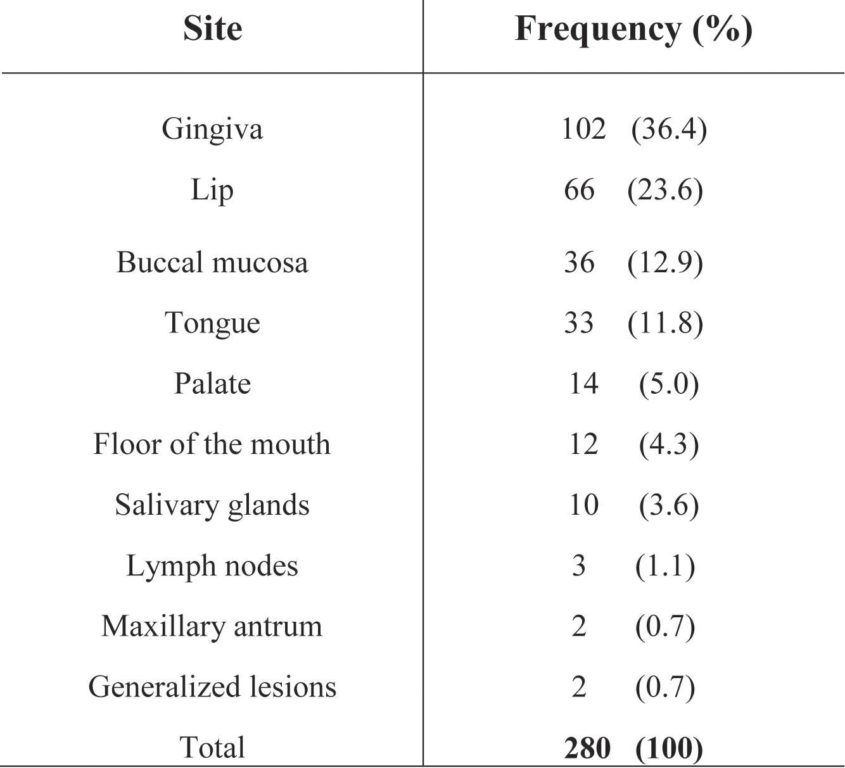 Table 2: Distribution of lesions relative to oral sites
Table 2: Distribution of lesions relative to oral sites
lesions (including benign and malignant salivary gland tumors; 26.8%) (Table 1). Lesions were generally more common in females except epithelial alterations and vascular lesions (Table 1). However there was no statistical significant difference in the gender distribution of lesions (Pearson Chi square = 9.87; P = 0.195)nor in the distribution of lesions between the different age groups (Pearson Chi square = 18.90; P = 0.579)
Reactive lesions accounted for the largest group of lesions and comprised mainly pyogenic granuloma and fibroma. Three-fifth (60%) of these lesions occurred in the gingiva followed by the buccal mucosa (15%) and tongue (13%). The salivary gland lesions were the second most common. Thisheterogeneousgroup of lesions constituted 26 % of total biopsies. A disproportionate amount of these lesions were located in the lips (62%) with the floor of the mouth a distant second (16%) followed by major salivary glands (11%). Mucous extravasation phenomenon (76%) was by far the dominant lesion followed by chronic sialadenitis (10%). All cases of the former that were seen occurred on the lower lip. Mucoepidermoid carcinoma and pleomorphic adenoma found in 3 patients (4%) were the only salivary gland tumors seen (Table 3).
Benign tumors of non-salivary gland origin accounted for 18 cases (6.4% of total biopsies). This rises to 31 cases (11% of total biopsies) if vascular benign tumors (hemangioma and lymphangioma) are added to this group as was done in many previous studies. The gingiva, buccal mucosa and tongue were the most commonly affected sites. The two most common were squamous papilloma and lymphangioma (Table 3).
As expected, malignant tumors were rarely seen in
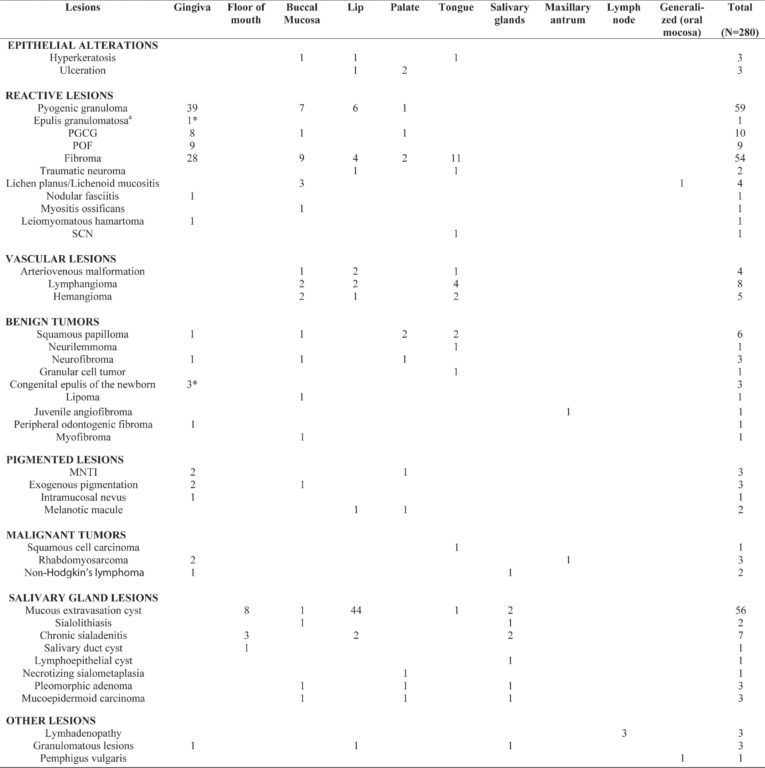 Table 3: Prevalence of individual lesions relative to their location
Table 3: Prevalence of individual lesions relative to their location
Abbreviations: PGCG, peripheral giant cell granuloma; POF, peripheral ossifying fibroma; MNTI, melanotic neuroectodermal tumor of infancy; SCN, solitary circumscribed neuroma.
aEpulis granulomatosa is an unusual for of pyogenic granuloma occurring in extraction sockets
Alveolar ridge
pediatric patients. Only six cases were found. They were mainly located on the gingiva (50%) with the remaining half distributed equally in 3 other oral sites. There were 3 cases of rhabdomyosarcoma, 2 cases of Non-Hodgkin’s lymphoma as well as a case of squamous cell carcinoma of the dorsal tongue (Table 3). Pigmented lesions were rare (9 cases in all) although it is noteworthy that in this
group of lesions, melanoticneuroectodermal tumor of infancy was well represented (3 cases) as a pigmented disorder seen commonly in infants.
DISCUSSION
This study reviewed the profile of oral soft tissue biopsies received and diagnosed in a University-based oral biopsy service in Saudi Arabia over a 30 year period.Due to the fact that there are no well-documented reports on pediatric oral diseases in the country as well as cultural and environmental differences which presumably may influence the pattern and prevalence of lesions in pediatric patients, studies like these are needed to help define future pediatric healthcare needs.
Previous studies, as in this study, have identified that the age-group most commonly associated with increased number of oral lesions in the pediatric age is the 6-12 year old group6,7,14. The differences seems to be much greater when the latter group are compared to the 0-5 years but rather attenuated when compared to those of 13-15 year old group or even older. This seemed to underline the continuous role being played by dentition in the evolution of some of the most common lesions. The mixed dentition stage is characterized by teeth resorption, crowding and even carious lesions which provides a good etiologic source (plaque and calculus accumulation, jagged teeth) for the reactive and inflammatory soft tissue lesions21. This may reduce slightly, albeit not significantly, as the permanent dentition comes into play in the older age groups. Moreover, to again emphasize the effect of the mixed dentition stage of tooth development regarding reactive and inflammatory lesions, some lesions which are exclusive to infants and children less than 5 year old who have not yet reached mixed dentition stageare tumors (e.g. congenital epulis, melanoticneuroectodermal tumor of infancy) and not reactive lesions.
Like in most previous studies, the most common lesions are the reactive lesions which constituted 51% of the total lesions in this study. However, in African children the most prevalent lesions were neoplastic9,possibly due to oversized role of some tumors such as Burkitt’s lymphoma that are environmentally endemic in sub-Saharan Africa22. Pyogenic granuloma and fibroma were by far the two most common lesions among the reactive lesions. As alluded to previously, trauma and chronic irritation (often as a result of the presence of gradually changing dentition) are the main etiologic sources of these lesions23.Gultekin et al (2003)7found giant cell granuloma as the most prevalent reactive lesion in their study of the Turkish population. Regarding the location of these lesions, the great majority were found on the gingiva. Fibromas were reported to accounted for 36% of such lesions. It is probable that in many studies, vascular anomaly has been reported under hemangioma, as often some pathologists still refer to vascular malformation as a form of hemangioma25. It is also probable that lymphangioma may also probably be more commonin Saudi children. It is noteworthy that apart from lesions associated with infancy (melanoticneuroectodermal tumor of infancy and congenital epulis),lymphangioma had the lowest mean age among the other lesions (Table 4).
In virtually all previous studies, benign tumors vastly
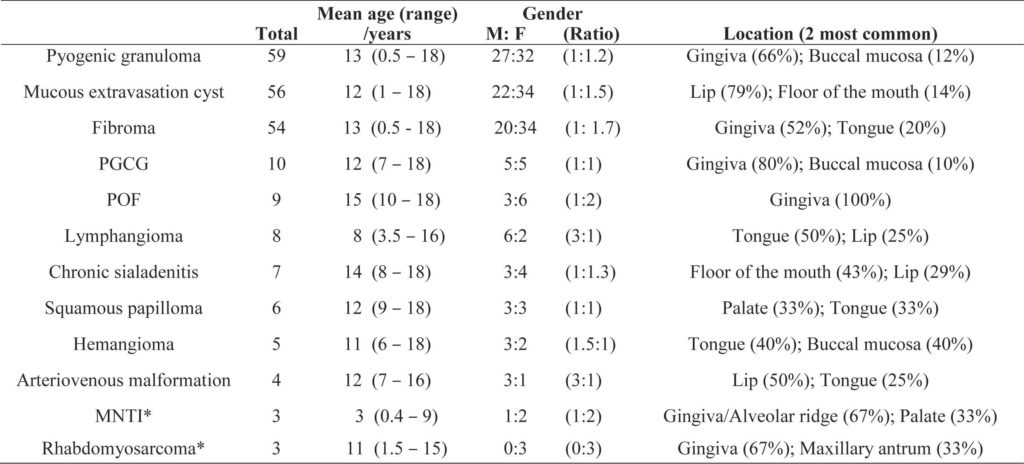 Table 4: Profile of the 12 most common lesions
Table 4: Profile of the 12 most common lesions
Abbreviations: PGCG, peripheral giant cell granuloma; POF, peripheral ossifying fibroma; MNTI, melanotic neuroectodermal tumor of infancy
*These lesions were selected randomly from other lesions having the same prevalence
be more commonly found in the buccal mucosa in Thai children6.
Vascular lesions were in general fairly common in this study, being the fourth most common group. In many studies despite being classified as benign non-odontogenic tumor, hemangioma tends to be relatively very common in pediatric patients and may even sometimes be almost as common as reactive lesions, while lymphangiomas are much less common1,6,7,14,24. In this study however, lymphangioma was more common than hemangioma. In addition, in previous studies arteriovenous malformation were rarely found in children.Jones and Franklin 2006 reported that vascular anomalies constituted 8% of connective tissue lesions in children while hemangioma outnumber malignant tumors in pediatric patients. The main reason is that the range and pattern of benign tumors that may be seen in pediatric patients is wide compared to the very narrow range of malignant tumors1,6,7. In this study, benign tumors are 3 times likely to be encountered than malignant tumors, and if neoplastic vascular lesions are added as was done in some studies, then the benign tumors are at least 5 times as common as malignant tumors. Although this is less than in most studies where the ratio ranged from 8:1 (benign:malignant)7 to as much as 29:16, it is difficult to compare studies in this area as most of them included salivary gland tumors, hard tissue tumors and odontogenic tumors. Rhabdomyosarcoma (especially the embryonal variant)is a malignant tumor often encountered in pediatric patients.All three cases in this study were embryonal. Squamous cell carcinoma of the dorsal tongue is very rare in comparison to ventral and lateral tongue in all studies on adult populations. The single case in an unusual site seen in this study probably underlines a relative difference in the etiologic source from cases commonly seen in the adult population. Generally in the adult population, majority of oral squamous cell carcinoma are related to tobacco and alcohol use.
In the very few previous studies that classify salivary gland lesions as a separate entity8,15 the findings were generally similar to the present study. Mucous extravasation cyst and chronic sialadenitis appear to be the two most common lesions. Tumors of salivary glands are rather uncommon but when diagnosed, are more likely to be pleomorphic adenoma if benign,and mucoepidermoid carcinoma when malignant.
In conclusion, this study reviewed the range of lesions seen in biopsies obtained from pediatric patients in a Saudi teaching hospital. Although it cannot claim to represent the actual prevalence of the diagnostic entities making up the soft tissue lesions because the setting is university teaching hospital, it has shown the range of lesions that should be expected by the clinician when sending a biopsy from pediatric patients for histopathology. As in most previous studies, most lesions in pediatric patients are reactive and benign but the clinician ought to be aware that malignant lesions maybe sometimes encountered. In addition, based on this study, it appears that lymphangioma may be relatively more common in Saudi patients.
REFERENCES
- Wang YL, Chang HH, Chang JY, Huang GF, Guo MK. Retrospective survey of biopsied oral lesions in pediatric patients. J Formos Med Assoc. 2009;108:862871.
- Rachidi S, Sood AJ, Patel KG, et al. Melanotic Neuroectodermal Tumor of Infancy: A Systematic Review. J Oral Maxillofac Surg. 2015.
- Conrad R, Perez MC. Congenital granular cell epulis. Arch Pathol Lab Med. 2014;138:128-131.
- Chen YK, Lin LM, Huang HC, Lin CC, Yan YH. A retrospective study of oral and maxillofacial biopsy lesions in a pediatric population from southern Taiwan. Pediatr Dent. 1998;20:404-410.
- Das S, Das AK. A review of pediatric oral biopsies from a surgical pathology service in a dental school. Pediatr Dent. 1993;15:208-211.
- Dhanuthai K, Banrai M, Limpanaputtajak S. A retrospective study of paediatric oral lesions from Thailand. Int J Paediatr Dent. 2007;17:248-253.
- Gultelkin SE, Tokman B, Turkseven MR. A review of paediatric oral biopsies in Turkey. Int Dent J. 2003;53:26-32.
- Jones AV, Franklin CD. An analysis of oral and maxillofacial pathology found in children over a 30-year period. Int J Paediatr Dent. 2006;16:19-30.
- Lawoyin JO. Paediatric oral surgical pathology service in an African population group: a 10 year review. Odontostomatol Trop. 2000;23:27-30.
- Lima Gda S, Fontes ST, de Araujo LM, Etges A, Tarquinio SB, Gomes AP. A survey of oral and maxillofacial biopsies in children: a single-center retrospective study of 20 years in Pelotas-Brazil. J Appl Oral Sci. 2008;16:397-402.
- Shah SK, Le MC, Carpenter WM. Retrospective review of pediatric oral lesions from a dental school biopsy service. Pediatr Dent. 2009;31:14-19.
- Skinner RL, Davenport WD, Jr., Weir JC, Carr RF. A survey of biopsied oral lesions in pediatric dental patients. Pediatr Dent. 1986;8:163-167.
- Sousa FB, Etges A, Correa L, Mesquita RA, de Araujo NS. Pediatric oral lesions: a 15-year review from Sao Paulo, Brazil. J Clin Pediatr Dent. 2002;26:413-418.
- Zuniga MD, Mendez CR, Kauterich RR, Paniagua DC. Paediatric oral pathology in a Chilean population: a 15-year review. Int J Paediatr Dent. 2013;23:346-351.
- Krolls SO, Trodahl JN, Boyers RC. Salivary gland lesions in children. A survey of 430 cases. Cancer. 1972;30:459-469.
- Blackwood HJ. Odontogenic tumours in the child. Br Dent J. 1965;119:431-438.
- Qannam A. Odontogenic tumors in children and adolescents: a 25 year’s retrospective study in Saudi population. Egypt Dent J. 2010;56:191-196.
- Jones JH. Non-odontogenic oral tumours in children. Br Dent J. 1965;119:439-447.
- Majorana A, Bardellini E, Flocchini P, Amadori F, Conti G, Campus G. Oral mucosal lesions in children from 0 to 12 years old: ten years’ experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e1318.
- Bessa CF, Santos PJ, Aguiar MC, do Carmo MA. Prevalence of oral mucosal alterations in children from 0 to 12 years old. J Oral Pathol Med. 2004;33:17-22.
- Gianelly AA. Crowding: timing of treatment. Angle Orthod. 1994;64:415-418.
- Walusansa V, Okuku F, Orem J. Burkitt lymphoma in Uganda, the legacy of Denis Burkitt and an update on the disease status. Br J Haematol. 2012;156:757-760.
- Jafarzadeh H, Sanatkhani M, Mohtasham N. Oral pyogenic granuloma: a review. J Oral Sci. 2006;48:167175.
- Lei F, Chen JY, Lin LM, et al. Retrospective study of biopsied oral and maxillofacial lesions in pediatric patients from southern Taiwan. J Dent Sci. 2013. 25. Redondo P. Vascular malformations (I). Concept, classification, pathogenesis and clinical features. Actas Dermosifiliogr. 2007;98:141-158.

